The Most Common Sleep Disorders and How to Treat Them
Understanding Insomnia and its Treatment Options
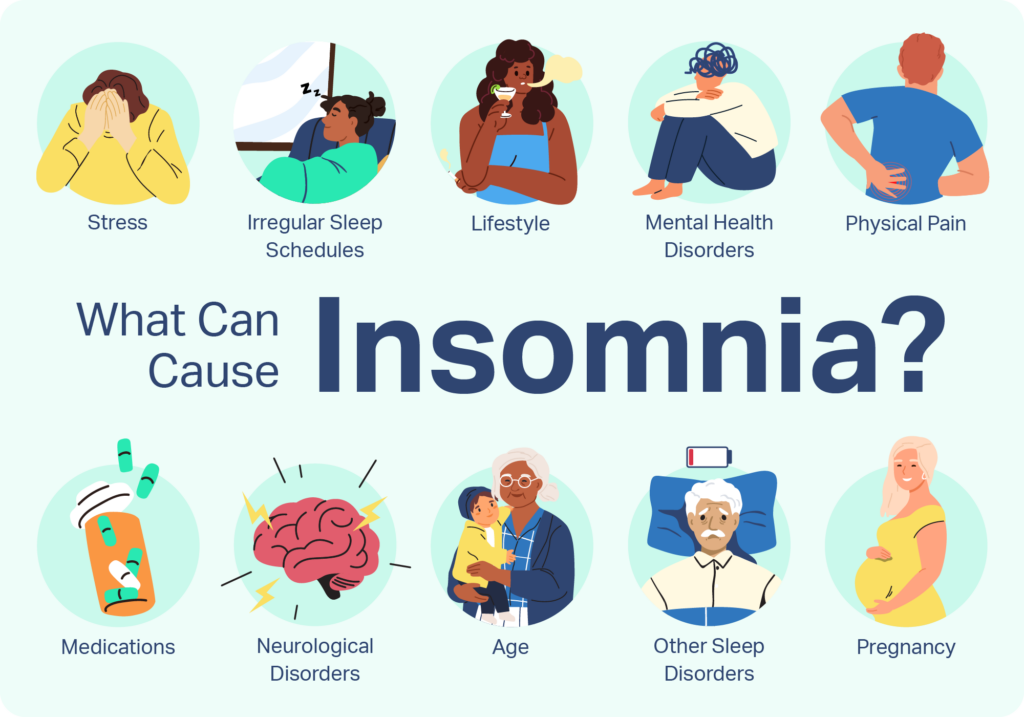
Insomnia, a common sleep disorder, affects millions of people worldwide. It is characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep. This can lead to daytime fatigue, irritability, and impaired functioning. Insomnia can be classified as acute (short-term) or chronic (lasting longer than three months), with various underlying causes.
There are several treatment options available for individuals struggling with insomnia. Non-pharmacological approaches include cognitive behavioral therapy for insomnia (CBT-I), which aims to address the thoughts and behaviors that contribute to sleep difficulties. CBT-I involves strategies such as sleep restriction, stimulus control, and relaxation techniques. Additionally, sleep hygiene practices, such as maintaining a consistent sleep schedule, creating a calm sleep environment, and avoiding stimulating activities before bedtime, can also be helpful. In some cases, medication may be prescribed short-term to alleviate symptoms and promote better sleep. It is important to consult with a healthcare professional to determine the most appropriate treatment approach based on individual needs.
Exploring the Causes and Treatments for Sleep Apnea
Sleep apnea is a common sleep disorder that affects millions of individuals worldwide. This condition is characterized by pauses in breathing or shallow breathing during sleep, which can lead to disrupted sleep patterns and various health issues. There are different types of sleep apnea, with obstructive sleep apnea (OSA) being the most prevalent form.
One of the primary causes of OSA is the relaxation of the throat muscles, leading to a blockage of the airway. This blockage can occur due to factors such as obesity, enlarged tonsils, or structural abnormalities in the airway. Additionally, certain lifestyle choices and habits, such as smoking and alcohol consumption, can contribute to the development of sleep apnea.
Treatment options for sleep apnea aim to restore regular breathing patterns during sleep and improve overall sleep quality. Continuous Positive Airway Pressure (CPAP) therapy is often recommended as a highly effective treatment for OSA. This involves wearing a mask that delivers a constant flow of air pressure, keeping the airway open and preventing pauses in breathing. Other treatment options include oral appliances, which help to reposition the jaw and tongue to maintain an open airway, and surgical interventions for individuals with severe cases of sleep apnea.
It is crucial for individuals experiencing symptoms of sleep apnea to seek medical attention, as this condition can have serious health consequences if left untreated. A healthcare professional can conduct a comprehensive evaluation and provide appropriate treatment options tailored to each individual’s needs. With the right management strategies, individuals with sleep apnea can improve their quality of sleep and reduce the risks associated with the condition.
The Impact of Restless Leg Syndrome on Sleep Quality and Available Treatments
Restless Leg Syndrome (RLS) is a neurological disorder that affects sleep quality in many individuals. The characteristic symptom of RLS is an irresistible urge to move the legs, often accompanied by uncomfortable sensations such as tingling, creeping, or pulling. These sensations worsen at rest and are temporarily relieved by movement, making it particularly challenging for individuals to fall asleep and maintain a restful sleep throughout the night.
The impact of RLS on sleep quality cannot be underestimated. Studies have found that individuals with RLS experience significant sleep disturbances, including difficulty falling asleep, frequent awakenings during the night, and reduced total sleep time. These disruptions can lead to daytime fatigue, increased daytime sleepiness, and overall decreased quality of life. The lack of quality sleep can also have a debilitating effect on cognitive function, mood, and overall mental health.
Fortunately, there are treatment options available to mitigate the impact of RLS on sleep quality. Medications such as dopamine agonists, benzodiazepines, and opioids have been shown to provide relief from RLS symptoms and improve sleep outcomes. Additionally, lifestyle modifications such as regular exercise, avoiding certain triggers like caffeine and tobacco, and practicing good sleep hygiene can also contribute to better sleep quality for individuals with RLS.
References:
1. Allen R, Picchietti D, Hening WA, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4(2):101-119.
2. Trenkwalder C, Benes H, Grote L, et al. Cabergoline compared to levodopa in the treatment of patients with severe restless legs syndrome: results from a multi-center, randomized, active controlled trial. Mov Disord. 2007;22(5):696-703.
Sleepwalking: Causes, Risks, and Strategies for Management
Sleepwalking, also known as somnambulism, is a parasomnia disorder characterized by complex behaviors and actions performed during sleep. The exact causes of sleepwalking are not yet fully understood, but research suggests that it may be linked to a variety of factors. One possible cause is genetic predisposition, as sleepwalking tends to run in families. Certain medications, such as sedatives and hypnotics, may also increase the likelihood of sleepwalking episodes. Furthermore, sleep deprivation, irregular sleep schedules, and underlying sleep disorders, such as sleep apnea or restless leg syndrome, have been associated with an increased risk of sleepwalking.
While sleepwalking itself may not be harmful, it does pose risks and potential dangers. Sleepwalkers can unknowingly leave their homes and wander into unsafe situations, such as traffic or other hazardous environments. They may also engage in behaviors that could result in injuries, such as falling down stairs or tripping on objects. Therefore, it is crucial for individuals who sleepwalk to take necessary precautions to ensure their safety and the safety of those around them.
Management strategies for sleepwalking typically involve creating a safe sleeping environment and implementing lifestyle modifications. Removing any potential hazards, such as sharp objects or furniture that could cause injury, from the sleepwalker’s vicinity can help minimize risks. Additionally, maintaining a consistent sleep schedule, practicing good sleep hygiene, and reducing stress levels may contribute to a reduction in sleepwalking episodes. In some cases, medication may be prescribed to help regulate sleep patterns and prevent sleepwalking. However, it is important to consult with a healthcare professional before starting any medication regimen.
In conclusion, sleepwalking is a complex sleep disorder that can have potential risks and dangers. While its exact causes are still being studied, genetics, medications, sleep deprivation, and underlying sleep disorders are believed to play a role. Managing sleepwalking episodes requires implementing safety measures and promoting healthy sleep habits. Consulting with a healthcare professional is vital for proper diagnosis and guidance on the most effective management strategies for each individual.
Uncovering the Causes and Remedies for Narcolepsy
Narcolepsy is a neurological disorder that affects approximately 1 in every 2,000 people worldwide. It is characterized by excessive sleepiness, sudden loss of muscle tone (known as cataplexy), sleep paralysis, and vivid hallucinations. While the exact cause of narcolepsy is still not fully understood, researchers believe that it may be a result of a combination of genetic and environmental factors.
One of the key factors believed to contribute to narcolepsy is the deficiency of a neurotransmitter called hypocretin, also known as orexin. Hypocretin helps regulate wakefulness and sleep by controlling the sleep-wake cycle. In individuals with narcolepsy, there is a significant reduction in the production of hypocretin, leading to disruptions in the normal sleep patterns.
Currently, there is no known cure for narcolepsy. However, there are various treatment options available to help manage the symptoms and improve the quality of life for individuals with this condition. The primary goal of treatment is to control excessive daytime sleepiness and minimize the occurrence of cataplexy episodes. This can be achieved through a combination of medication, lifestyle modifications, and behavioral therapy. Medications such as stimulants, antidepressants, and sodium oxybate are commonly prescribed to promote wakefulness and reduce the frequency of cataplexy attacks. Additionally, adopting good sleep hygiene practices, maintaining a regular sleep schedule, and managing stress levels can also play a crucial role in symptom management.
The Intricacies of Sleep Paralysis: Causes and Coping Mechanisms
Sleep paralysis is a phenomenon that occurs during the sleep-wake transition, where the individual is temporarily unable to move or speak. This can be an incredibly distressing experience, as it may be accompanied by vivid hallucinations and a sense of pressure on the chest. Although sleep paralysis is relatively common, affecting about 8% of the general population, its exact causes are still not fully understood.
Several factors have been identified as potential triggers for sleep paralysis. One common cause is sleep deprivation, which can disrupt the sleep cycle and increase the likelihood of experiencing an episode. Another contributing factor is a disruption in the normal REM sleep patterns, with sleep paralysis often occurring when individuals transition into or out of REM sleep. Additionally, there is evidence to suggest that sleep paralysis may be more prevalent in individuals with certain sleep disorders, such as narcolepsy. Understanding the underlying causes of sleep paralysis is crucial for developing effective coping mechanisms and treatment strategies.
Here’s a short data table covering the intricacies of sleep paralysis, including causes and coping mechanisms:
| Intricacies of Sleep Paralysis | Key Concepts | Credible Source |
|---|---|---|
| Sleep Paralysis Definition | A temporary inability to move or speak while falling asleep or waking up. | Mayo Clinic – Sleep Paralysis |
| Causes and Triggers | Linked to sleep deprivation, irregular sleep patterns, and certain sleep disorders. | Sleep Foundation – Sleep Paralysis Causes |
| Association with REM Sleep | Often occurs during transitions in and out of rapid eye movement (REM) sleep. | National Institute of Neurological Disorders and Stroke – Sleep Paralysis |
| Coping Mechanisms | Focus on improving sleep hygiene, maintaining a consistent sleep schedule, and managing stress. | American Academy of Sleep Medicine – Sleep Paralysis |
Examining the Relationship Between Anxiety and Sleep Disorders

Anxiety and sleep disorders often go hand in hand, creating a challenging cycle for those affected. While it is natural to feel anxious from time to time, chronic anxiety can disrupt sleep patterns, leading to a variety of sleep disorders. On the other hand, sleep disorders can also trigger or aggravate anxiety symptoms, making it crucial to understand the relationship between the two and explore effective management strategies.
Research suggests that the relationship between anxiety and sleep disorders is bidirectional. Anxiety can lead to insomnia, characterized by difficulty falling asleep, staying asleep, or both. This can be attributed to the constant worry, racing thoughts, and physical tension associated with anxiety. Conversely, sleep disturbances, such as sleep apnea or restless leg syndrome, can increase anxiety levels due to the impact on sleep quality and overall daytime functioning. Understanding this intricate relationship can help individuals and healthcare professionals develop comprehensive treatment plans that address both anxiety and sleep disorders simultaneously.
Understanding the Effects of Depression on Sleep and Available Treatment Approaches
Depression can have a significant impact on a person’s sleep patterns, often leading to chronic insomnia or excessive daytime sleepiness. Individuals suffering from depression may find it difficult to fall asleep or experience frequent awakening throughout the night. Sleep quality is compromised, resulting in daytime fatigue and reduced performance in daily activities.
Various treatment approaches are available to address the effects of depression on sleep. One commonly recommended intervention is cognitive-behavioral therapy for insomnia (CBT-I). This therapy aims to identify and modify maladaptive thoughts and behaviors that contribute to sleep disturbances. By addressing negative thought patterns and implementing healthy sleep practices, CBT-I can improve sleep outcomes and reduce depressive symptoms. Additionally, medications such as selective serotonin reuptake inhibitors (SSRIs) are often prescribed to manage both depression and sleep disturbances, as they can promote more restful sleep.
It is crucial to recognize the reciprocal relationship between depression and sleep disturbances. While depression can disrupt sleep patterns, poor sleep can also exacerbate depressive symptoms. By understanding the effects of depression on sleep and utilizing available treatment approaches, individuals can enhance their sleep quality and overall well-being. Further research and clinical trials are ongoing to develop innovative therapies that target both depression and sleep disturbances, highlighting the importance of a multidisciplinary approach to this complex issue.
Exploring the Causes and Solutions for Bruxism (Teeth Grinding)
Bruxism, commonly known as teeth grinding, is a condition that affects many individuals, causing them to clench or grind their teeth involuntarily, often during sleep. The causes of bruxism are multifactorial and can vary from person to person. One of the primary causes is believed to be stress and anxiety, which can lead to increased muscle tension in the jaw. Other potential factors include misalignment of the teeth, an abnormal bite, or certain medical conditions such as temporomandibular joint disorder (TMJ).
Finding effective solutions for bruxism is essential to prevent further damage to the teeth and alleviate associated symptoms. Treatment options generally focus on minimizing stress and muscle tension in the jaw. One common approach is the use of night guards or splints, custom-made devices worn during sleep to protect the teeth from grinding. Additionally, stress management techniques such as relaxation exercises, counseling, and even cognitive behavioral therapy may be beneficial. In some cases, addressing the underlying dental or skeletal issues through orthodontic or dental work may also be considered to alleviate bruxism symptoms.
The Connection Between Sleep Disorders and Chronic Pain: Strategies for Relief
Sleep disorders and chronic pain often go hand in hand, creating a vicious cycle that can significantly impact an individual’s quality of life. On one hand, sleep disorders such as insomnia and sleep apnea can lead to disrupted sleep patterns and inadequate rest, making it more challenging for the body to recover from chronic pain. On the other hand, chronic pain can make it difficult to fall asleep or stay asleep, leading to further sleep disturbances.
Addressing the connection between sleep disorders and chronic pain requires a comprehensive approach that combines strategies to manage both aspects effectively. One such strategy is the implementation of good sleep hygiene practices. This includes maintaining a consistent sleep schedule, creating a sleep-friendly environment, and avoiding stimulants close to bedtime. By establishing a regular sleep routine and creating an optimal sleep environment, individuals may improve their chances of obtaining quality sleep, which can help alleviate chronic pain symptoms.
Additionally, cognitive-behavioral therapy for insomnia (CBT-I) has shown promising results in managing both sleep disorders and chronic pain. CBT-I focuses on identifying and addressing the underlying thoughts and behaviors that contribute to insomnia. Through a combination of relaxation techniques, sleep restriction, and cognitive restructuring, individuals can develop healthier sleep patterns and learn strategies to cope with chronic pain more effectively.
It is important to approach the treatment of sleep disorders and chronic pain holistically, considering both physical and psychological factors. By combining various strategies such as sleep hygiene practices and cognitive-behavioral therapy, individuals can break the cycle of sleep disturbances and chronic pain, leading to improved overall well-being.
Addressing the Challenges of Shift Work Sleep Disorder
Shift work sleep disorder (SWSD) is a condition that affects individuals who work non-traditional hours, such as evening, night, or rotating shifts. The challenges associated with this disorder can significantly impact an individual’s overall well-being and quality of life. One of the key challenges faced by those with SWSD is the disruption of their natural sleep-wake cycle, which can lead to difficulties falling asleep or staying asleep during the appropriate hours.
Managing SWSD can be particularly challenging due to the unique demands of shift work. Individuals with this disorder often struggle to maintain a consistent sleep schedule, as their work schedule frequently changes. Additionally, the work environment itself, with its noise, bright lights, and irregular routines, can further impede sleep quality. These challenges can cause excessive sleepiness, decreased alertness, and significant fatigue, which can affect job performance, safety, and overall health. Finding effective strategies to address the challenges of SWSD is crucial for individuals who work non-traditional hours to improve their sleep quality and mitigate the negative effects of the disorder.
Exploring the Causes and Management of REM Sleep Behavior Disorder
REM sleep behavior disorder (RBD) is a sleep disorder characterized by the absence of muscle paralysis during the rapid eye movement (REM) stage of sleep. This results in individuals acting out vivid and sometimes violent dreams, often posing a risk to themselves and their bed partners. While the exact causes of RBD remain unclear, studies suggest that it may be associated with neurological conditions such as Parkinson’s disease or olfactory dysfunction.
Treatment options for RBD aim to manage the symptoms and reduce the risk of injury. One of the most common approaches is the use of medication, particularly clonazepam, which acts as a sedative and helps suppress muscle movements during sleep. However, it is important to find the lowest effective dose to avoid potential side effects such as daytime sedation. Other non-pharmacological strategies may include maintaining a safe sleep environment by removing sharp objects, padding the bed, and using bed alarms to alert the individual to wakefulness during episodes. Additionally, cognitive-behavioral therapy (CBT) is often recommended to address any underlying psychological factors that may contribute to the development or exacerbation of RBD. CBT can help individuals develop coping mechanisms and relaxation techniques to minimize the occurrence and intensity of RBD episodes.
As research continues to unravel the complexities of REM sleep behavior disorder, healthcare professionals are gaining a better understanding of its causes and improving management strategies. By combining medical interventions with behavioral therapies, individuals with RBD can find relief and enjoy safer and more restful sleep, enhancing their overall quality of life.
The Impact of Sleep Disorders on Children and Available Treatment Options.
Sleep disorders can have a significant impact on children, affecting both their physical and mental well-being. One common sleep disorder in children is insomnia, which can lead to difficulty falling asleep, staying asleep, or experiencing quality sleep. Insomnia in children can result from various factors, such as anxiety, stress, or medical conditions. The consequences of insomnia in children can be far-reaching, including daytime sleepiness, impaired concentration, mood disturbances, and decreased academic performance.
Fortunately, there are a range of treatment options available to help address sleep disorders in children. These options may include behavioral interventions, such as establishing a consistent sleep routine or practicing relaxation techniques before bedtime. Additionally, medication may be prescribed in certain cases to help regulate the sleep-wake cycle. It is important for parents and caregivers to work closely with healthcare professionals to determine the most appropriate treatment plan for their child’s specific sleep disorder. By addressing sleep disorders in children, we can help promote healthy sleep habits and improve overall well-being.
What are the common sleep disorders in children?
Common sleep disorders in children include insomnia, sleep apnea, restless leg syndrome, sleepwalking, narcolepsy, sleep paralysis, anxiety-related sleep disorders, depression-related sleep disturbances, bruxism (teeth grinding), and chronic pain-related sleep disorders.
How is insomnia treated in children?
Insomnia in children can be treated through various methods such as improving sleep hygiene, cognitive-behavioral therapy, relaxation techniques, and medication in some cases.
What causes sleep apnea in children?
Sleep apnea in children can be caused by a variety of factors including enlarged tonsils or adenoids, obesity, craniofacial abnormalities, or genetic conditions.
What are the available treatments for sleep apnea in children?
Treatment options for sleep apnea in children may include the removal of tonsils or adenoids, continuous positive airway pressure (CPAP) therapy, dental appliances, weight management, or surgery in severe cases.
What impact does restless leg syndrome have on sleep quality in children?
Restless leg syndrome can greatly affect sleep quality in children, leading to difficulties falling asleep or staying asleep, as well as daytime fatigue or irritability.
How can restless leg syndrome be treated in children?
Treatment options for restless leg syndrome in children may include lifestyle changes, iron supplements (if iron deficiency is present), medications, or other therapies recommended by a healthcare professional.
What are the causes and risks associated with sleepwalking in children?
The causes of sleepwalking in children may vary, but it can be triggered by factors such as sleep deprivation, certain medications, fever, or underlying sleep disorders. Risks associated with sleepwalking include potential injuries from wandering or engaging in unsafe activities while asleep.
What strategies can be used to manage sleepwalking in children?
Strategies for managing sleepwalking in children include establishing a regular sleep routine, creating a safe sleep environment, implementing safety measures, and consulting with a healthcare professional for further guidance.
What are the causes of narcolepsy in children?
The exact cause of narcolepsy in children is not fully understood, but it is believed to involve a combination of genetic and environmental factors.
How is narcolepsy treated in children?
Treatment for narcolepsy in children typically involves a combination of medication, lifestyle adjustments, and counseling to manage symptoms and improve daily functioning.
What are the causes of sleep paralysis in children?
Sleep paralysis in children can be caused by disruptions in the sleep-wake cycle, sleep deprivation, irregular sleep schedules, stress, or anxiety.
How can children cope with sleep paralysis?
Coping mechanisms for children experiencing sleep paralysis may include maintaining a consistent sleep schedule, practicing relaxation techniques, reducing stress, and implementing good sleep hygiene practices.
Is there a link between anxiety and sleep disorders in children?
Yes, anxiety can contribute to the development or worsening of sleep disorders in children. The relationship between anxiety and sleep disorders is complex and may require a multidisciplinary approach for effective management.
How does depression affect sleep in children?
Depression can disrupt sleep patterns in children, leading to difficulties falling asleep, staying asleep, or experiencing poor sleep quality. It can also contribute to excessive daytime sleepiness or fatigue.
What treatment approaches are available for sleep disturbances related to depression in children?
Treatment approaches for sleep disturbances related to depression in children may include therapy, medication, lifestyle changes, and the management of underlying depressive symptoms.
What causes bruxism (teeth grinding) in children?
The exact cause of bruxism in children is not fully understood, but it can be associated with factors such as stress, anxiety, abnormal bite, or certain medical conditions.
How is bruxism treated in children?
Treatment for bruxism in children may involve behavioral interventions, stress management techniques, dental interventions (e.g., mouthguards), or addressing underlying causes through medical or psychological interventions.
What is the connection between sleep disorders and chronic pain in children?
Sleep disorders and chronic pain can often coexist in children, with one condition exacerbating the other. Chronic pain can impact sleep quality, while sleep disturbances can amplify pain perception.
What strategies can be used to find relief from sleep disorders related to chronic pain in children?
Strategies for finding relief from sleep disorders related to chronic pain in children may involve a combination of pain management techniques, sleep hygiene practices, relaxation techniques, and consultation with healthcare professionals specializing in both sleep and pain disorders.
How does shift work affect sleep in children?
Shift work can significantly disrupt sleep patterns in children, as it often involves irregular or nighttime schedules that conflict with the body’s natural sleep-wake rhythms.
What are the challenges associated with shift work sleep disorder in children?
Challenges associated with shift work sleep disorder in children may include difficulties falling asleep or staying asleep during unconventional hours, increased daytime sleepiness, and potential impact on overall well-being and cognitive functioning.
How can shift work sleep disorder in children be addressed?
Addressing shift work sleep disorder in children may require implementing strategies such as creating a sleep-friendly environment, establishing consistent sleep routines, optimizing light exposure, and seeking specialized guidance from healthcare professionals.
How is REM sleep behavior disorder managed in children?
Management of REM sleep behavior disorder in children may involve safety measures to minimize the risk of injury during episodes, addressing underlying causes or triggers, and potentially utilizing medication or other therapies under the guidance of healthcare professionals.
What treatment options are available for sleep disorders in children?
Treatment options for sleep disorders in children may vary depending on the specific disorder and its underlying causes. They can include lifestyle changes, behavioral interventions, medication, therapy, or a combination of approaches tailored to the individual child’s needs.