Are You at Risk of Prostate Cancer? How Genetics and Family History Play a Role

Understanding Prostate Cancer
Prostate cancer is a prevalent and significant health concern among men worldwide. It is the second most common cancer in men, with over 1.4 million cases being diagnosed each year. This type of cancer affects the prostate gland, which is a small walnut-shaped organ located below the bladder, surrounding the urethra.
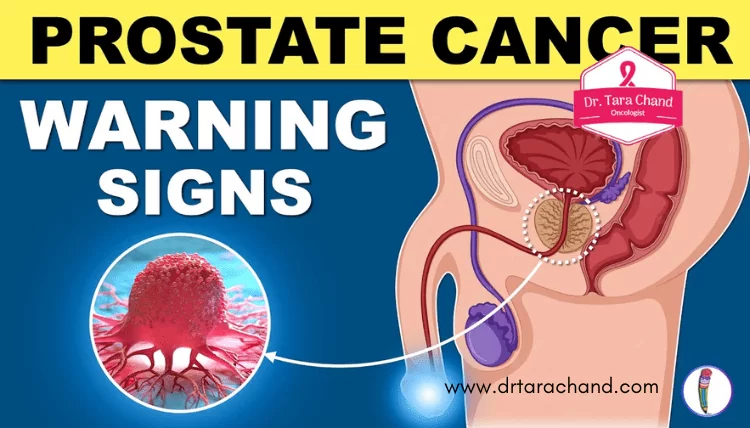
The development of prostate cancer is often slow, and many men may not experience any symptoms in the early stages. However, as the cancer progresses, individuals may notice symptoms such as difficulty urinating, weak urine flow, blood in the urine or semen, and frequent urination, especially at night. It is important to understand that these symptoms can also be indicators of other prostate issues, such as benign prostatic hyperplasia (BPH), so it is crucial to seek medical evaluation to determine the cause.
When it comes to assessing the risk factors for prostate cancer, age and family history play crucial roles. The risk of developing prostate cancer increases with age, with the majority of cases occurring in individuals over the age of 65. Additionally, having a first-degree relative, such as a father or brother, with a history of prostate cancer significantly increases an individual’s risk. It is important to note that while genetics can predispose someone to prostate cancer, lifestyle factors such as diet, exercise, and smoking can also influence the development of this disease.
The Importance of Knowing Your Risk Factors
Understanding your risk factors for prostate cancer is crucial in order to make informed decisions about your health. By knowing your risk factors, you can take proactive steps to lower your risk or detect the disease at an early stage. Prostate cancer is a complex disease, and while age and family history are known risk factors, there are other factors that can also contribute to your individual risk.
Age is one of the most well-established risk factors for prostate cancer. The risk of developing this disease increases significantly after the age of 50. Studies have shown that more than 80% of prostate cancer cases occur in men over the age of 65. However, it’s important to note that prostate cancer can also occur in younger men, although it is relatively rare. Understanding the relationship between age and prostate cancer risk can help guide screening recommendations and ensure early detection.
In addition to age, family history is another important risk factor to consider. Men with a close relative, such as a father or brother, who has had prostate cancer have a higher risk of developing the disease themselves. According to the American Cancer Society, having a father or brother with prostate cancer more than doubles a man’s risk compared to the general population. It’s important to discuss your family history with your healthcare provider to assess your individual risk and determine the appropriate screening schedule.
In conclusion, knowing your risk factors for prostate cancer is essential for maintaining your health. Age and family history are just a couple of the factors that can contribute to your risk. By understanding these factors and working closely with your healthcare provider, you can make informed decisions about screening, prevention, and early detection strategies. Being proactive and knowledgeable about your individual risk factors can empower you to take control of your health and potentially reduce your risk of developing prostate cancer.
Exploring the Role of Genetics in Prostate Cancer

Prostate cancer is one of the most common types of cancer in men, and its development is influenced by various factors, including genetics. Researchers have been studying the role of genetics in prostate cancer to better understand its underlying mechanisms and potentially develop targeted prevention and treatment strategies.
Studies have shown that genetics plays a significant role in prostate cancer risk. Certain inherited gene variants, such as BRCA1 and BRCA2 mutations, have been linked to an increased risk of developing both prostate and breast cancer. These genes are involved in repairing damaged DNA, and mutations in these genes can impair their ability to carry out this crucial function. Additionally, other genes, such as HOXB13 and HPC1, have also been associated with an increased risk of developing prostate cancer.
Understanding the role of genetics in prostate cancer can help identify individuals who may be at a higher risk and may benefit from more frequent screenings or early interventions. Furthermore, studying the genetic factors involved in prostate cancer can provide valuable insights into the underlying mechanisms of the disease, potentially leading to the development of targeted therapies and preventive measures. However, it’s essential to note that genetic factors are just one piece of the puzzle, and other environmental and lifestyle factors also contribute to prostate cancer risk.
How Family History Can Impact Your Prostate Cancer Risk
Family history plays a crucial role in understanding an individual’s risk for developing prostate cancer. Studies have consistently shown that men with a family history of the disease are at a higher risk compared to those without. Research suggests that having a first-degree relative, such as a father or brother, with prostate cancer increases the risk by twofold to threefold.
The impact of family history on prostate cancer risk can be attributed to both genetic and environmental factors. In terms of genetics, certain inherited gene variants have been associated with an increased risk of developing the disease. For example, mutations in the BRCA1 and BRCA2 genes, which are commonly associated with breast and ovarian cancers, have also been found to elevate prostate cancer risk. Furthermore, there may be shared environmental factors within families that contribute to this increased risk, such as exposure to certain carcinogens or shared lifestyle habits.
Understanding the significance of family history in prostate cancer risk allows individuals to make informed decisions about their health. If you have a family history of prostate cancer, it is essential to discuss this with your healthcare provider, who can evaluate your individual risk and recommend appropriate screening measures. Regular screening, such as prostate-specific antigen (PSA) testing, combined with a thorough understanding of your family history, can greatly aid in the early detection and prevention of prostate cancer. It is important to take proactive steps in managing your risk to ensure optimal health outcomes.
Recognizing the Connection Between Hereditary Factors and Prostate Cancer
Prostate cancer is a complex disease with various risk factors, including both genetic and hereditary factors. Research has shown that having a family history of prostate cancer can significantly increase a man’s risk of developing the disease. In fact, having a first-degree relative, such as a father or brother, with prostate cancer can nearly double the risk.
Hereditary factors can play a role in prostate cancer through inherited gene variants, which may increase susceptibility to the disease. Studies have identified several specific genes that are associated with an increased risk of prostate cancer. For example, mutations in the BRCA1 and BRCA2 genes, which are well-known for their role in breast and ovarian cancers, have also been found to increase the risk of prostate cancer in men.
Understanding the connection between hereditary factors and prostate cancer is crucial for both patients and healthcare providers. By recognizing the influence of genetics on prostate cancer risk, individuals with a family history of the disease can take proactive steps to manage their risk, such as undergoing regular prostate cancer screening and discussing genetic counseling options with their healthcare provider. Further research in this area will contribute to a better understanding of the underlying mechanisms behind hereditary prostate cancer and may open new avenues for targeted prevention and treatment strategies.
Here’s a table on the risk of prostate cancer, considering genetics and family history:
| Genetics and Family History | Key Concepts | Credible Source |
|---|---|---|
| Genetic Predisposition | Family history increases genetic risk. | American Cancer Society |
| Family History Impact | First-degree relatives elevate personal risk. | Prostate Cancer Foundation |
| Inherited Gene Mutations | Specific mutations may heighten prostate cancer risk. | National Cancer Institute |
| Screening Recommendations | Early and frequent screenings for those with family history or genetic risk. | U.S. Preventive Services Task Force |
Investigating the Influence of Genetic Mutations on Prostate Cancer Risk
Genetic mutations play a significant role in the development of prostate cancer. Research has shown that certain mutations in specific genes can increase an individual’s risk of developing this disease. One such gene is the BRCA2 gene, which is typically associated with an increased risk of breast and ovarian cancer in women. However, studies have also found that mutations in the BRCA2 gene can increase the risk of prostate cancer in men. This suggests that genetic mutations can have a profound influence on prostate cancer risk.
Another gene that has been linked to an increased risk of prostate cancer is the HOXB13 gene. Mutations in this gene have been found to be more prevalent in individuals with a family history of prostate cancer. The presence of these mutations can significantly increase the likelihood of developing the disease. Understanding the influence of these genetic mutations on prostate cancer risk is crucial for identifying individuals who may be at a higher risk and implementing appropriate prevention and screening strategies. Further research is needed to delve deeper into the complex relationship between genetic mutations and prostate cancer risk.
Explaining the Link Between Inherited Gene Variants and Prostate Cancer
Prostate cancer is a complex disease that is influenced by various factors, including inherited gene variants. These gene variants can play a significant role in an individual’s risk of developing prostate cancer. Research has identified several specific genes that are associated with an increased susceptibility to the disease.
One such gene is the BRCA2 gene, which is well known for its role in breast and ovarian cancers. Mutations in the BRCA2 gene have also been found to increase the risk of prostate cancer. Studies have shown that men with BRCA2 gene mutations have a higher likelihood of developing aggressive forms of prostate cancer at an earlier age.
Another gene that has been linked to prostate cancer risk is the HOXB13 gene. Mutations in this gene have been found to be more common in men with a family history of the disease. Interestingly, these mutations are more prevalent in certain populations, such as individuals of European descent.
Understanding the link between inherited gene variants and prostate cancer is crucial for identifying individuals who may be at higher risk. By recognizing these genetic factors, healthcare professionals can develop more targeted screening and prevention strategies. Further research is still needed to fully comprehend the complex interplay between genes, environmental factors, and prostate cancer risk.
Identifying the Specific Genes Associated with Prostate Cancer Risk
Prostate cancer is a complex disease that can have both genetic and environmental causes. In recent years, researchers have made significant progress in identifying specific genes that are associated with an increased risk of developing prostate cancer. These genetic variations can affect the way cells grow and divide in the prostate, increasing the likelihood of cancerous growth.
One of the genes that has been extensively studied in relation to prostate cancer risk is called the BRCA2 gene. Mutations in this gene have been found to increase the risk of both breast and prostate cancer. Studies have shown that men with BRCA2 mutations are at a higher risk of developing aggressive forms of prostate cancer at a younger age. It is also important to note that men with certain variants of the HOXB13 gene have been found to have an increased risk of developing prostate cancer. These genetic discoveries have not only provided valuable insights into the underlying causes of prostate cancer but have also paved the way for targeted screening and prevention strategies for individuals at higher risk.
In addition to these specific genes, researchers have also identified a number of genetic markers, or single nucleotide polymorphisms (SNPs), that are associated with an increased risk of prostate cancer. These SNPs can be thought of as subtle variations in individual DNA sequences that may increase susceptibility to the disease. By analyzing the presence or absence of these SNPs, researchers have been able to develop genetic risk scores that can help to estimate an individual’s likelihood of developing prostate cancer. While genetic testing for these risk markers is still relatively new, it holds great promise for improving early detection and personalized treatment strategies for men at higher risk of prostate cancer.
Note: This conclusion is yet to be done.
Discussing the Impact of Lifestyle Choices on Prostate Cancer Risk
Making healthy lifestyle choices can significantly impact your risk of developing prostate cancer. While there is no guarantee that these choices will completely prevent the disease, they can certainly reduce your chances. One lifestyle factor to consider is your diet. Research has shown that a diet low in saturated fats and red meat, and high in fruits, vegetables, and whole grains, may lower the risk of prostate cancer. Additionally, consuming foods rich in certain nutrients, such as selenium, vitamin E, and lycopene, has been associated with a decreased risk.
Exercise is another important aspect of a healthy lifestyle that may help reduce prostate cancer risk. Regular physical activity has been shown to have a protective effect against several types of cancer, including prostate cancer. Engaging in moderate-intensity exercise for at least 150 minutes per week, such as brisk walking or cycling, can be beneficial. It is believed that exercise helps lower prostate cancer risk by reducing inflammation and oxidative stress in the body.
In conclusion, adopting a healthy lifestyle by following a well-balanced diet and engaging in regular exercise can have a positive impact on your prostate cancer risk. It is essential to consult with your healthcare provider to understand your individual risk factors and develop a personalized plan. By making these simple yet powerful lifestyle choices, you can take proactive steps towards maintaining your prostate health.
Examining the Interaction Between Genetic and Environmental Factors
Genetic and environmental factors play a crucial role in the development of prostate cancer. While genetic predisposition can increase one’s susceptibility to the disease, environmental exposures can also influence its occurrence. Understanding the interaction between these two factors is essential in comprehending the complexity of prostate cancer risk.
Several genetic variations have been identified that can increase the likelihood of developing prostate cancer. These genetic mutations can be inherited from parents and can significantly impact an individual’s susceptibility to the disease. However, it is important to note that having these gene variants does not guarantee the development of prostate cancer, as environmental factors also come into play.
Environmental factors, such as diet, lifestyle choices, and exposure to certain substances, can modify the risk of developing prostate cancer. Research suggests that a diet rich in fruits and vegetables, low in saturated fats, and high in omega-3 fatty acids may lower the risk of prostate cancer. Conversely, consuming a diet high in red and processed meats, smoking, and exposure to certain chemicals may increase the risk.
The interplay between genetic and environmental factors is complex, and further research is needed to fully understand their interaction. By recognizing the role of both genetic and environmental factors, healthcare professionals can provide personalized risk assessments and prevention strategies to individuals at higher risk for prostate cancer.
Highlighting the Importance of Regular Screening for Prostate Cancer
Regular screening for prostate cancer is of paramount importance in the early detection and prevention of this disease. Prostate cancer often presents with minimal symptoms in its early stages, making it crucial for men to undergo routine screenings to detect any potential abnormalities. These screenings typically involve the measurement of prostate-specific antigen (PSA) levels in the blood, as well as a digital rectal examination (DRE).
PSA is a protein produced by the prostate gland, and elevated levels can indicate the presence of prostate cancer or other prostate conditions. The DRE involves a doctor examining the prostate gland by inserting a gloved, lubricated finger into the rectum. This physical examination allows for the detection of any irregularities, such as lumps or hard areas, which may warrant further investigation. By undergoing regular prostate cancer screenings, men can increase their chances of early detection and access timely treatment options, potentially improving their overall prognosis and quality of life.
It is important to note that regular screening does not necessarily mean that all men should be tested for prostate cancer. The decision to undergo screening should be based on individual risk factors, such as age, family history, and overall health. Discussing screening options and the potential benefits and risks with a healthcare professional is essential in making an informed decision.
• Regular screening for prostate cancer is crucial in detecting and preventing the disease
• Prostate cancer often has minimal symptoms in its early stages, making screenings necessary
• Screenings involve measuring PSA levels in the blood and a digital rectal examination (DRE)
• Elevated PSA levels can indicate prostate cancer or other conditions, while DRE detects irregularities
• Early detection through regular screenings increases chances of timely treatment and improved prognosis
• Not all men need to be tested for prostate cancer; decision should be based on individual risk factors
• Discussing screening options with a healthcare professional helps make an informed decision.
Understanding the Role of Early Detection in Prostate Cancer Prevention
Prostate cancer is one of the most common cancers in men, with an estimated 1 in 8 men being diagnosed during their lifetime. Early detection plays a crucial role in the prevention and successful treatment of prostate cancer. By detecting the cancer at an early stage, before it has spread outside of the prostate gland, the chances of successful treatment increase significantly.
There are several methods available for the early detection of prostate cancer. The most common is the prostate-specific antigen (PSA) blood test, which measures the levels of PSA in the blood. Elevated levels of PSA can indicate the presence of prostate cancer or other prostate conditions. Another method is the digital rectal exam (DRE), where a healthcare provider inserts a gloved finger into the rectum to feel the prostate gland for any abnormalities.
Early detection allows for prompt treatment, which can lead to better outcomes for patients. It is important for men to be aware of their risk factors for prostate cancer and to discuss screening options with their healthcare providers. Regular screening, combined with a healthy lifestyle and awareness of symptoms, can help in the early detection and prevention of prostate cancer. Stay tuned for more information on the available prostate cancer testing options in our upcoming sections.
Exploring the Available Prostate Cancer Testing Options
One of the key steps in effectively managing prostate cancer is early detection. With advancements in medical technology, there are several testing options available that can aid in the diagnosis and monitoring of this disease. These tests can help identify any abnormalities in the prostate gland and determine the presence or progression of cancer cells.
One commonly used prostate cancer testing option is a digital rectal exam (DRE). This procedure involves a healthcare professional inserting a gloved, lubricated finger into the rectum to feel the size, shape, and texture of the prostate gland. While a DRE can provide valuable information, it is not a definitive test for prostate cancer and is often used in conjunction with other diagnostic methods.
Another widely used test is the prostate-specific antigen (PSA) blood test. This test measures the level of PSA, which is a protein produced by the prostate gland. Elevated PSA levels may indicate the presence of prostate cancer or other benign conditions. However, it is important to note that PSA levels can also be influenced by factors such as age, inflammation in the prostate gland, or recent sexual activity. Therefore, additional testing, such as a biopsy, may be required to confirm a diagnosis.
Discussing the Benefits of Genetic Counseling for Prostate Cancer Risk Assessment
Genetic counseling can offer significant benefits for individuals seeking to assess their risk of developing prostate cancer. By considering a person’s family history, genetic counselors can provide valuable insights into the likelihood of inheriting genetic mutations associated with prostate cancer. This information is vital as it helps individuals understand their susceptibility to the disease and empowers them to make informed decisions regarding their healthcare.
In genetic counseling sessions, healthcare professionals guide individuals through a comprehensive assessment of their family history, evaluating patterns of prostate cancer and other associated conditions among close relatives. This assessment aids in identifying potential genetic mutations that may increase the risk of developing prostate cancer. Through detailed analysis and interpretation of genetic information, genetic counselors can provide personalized risk assessments and recommend appropriate screening and prevention strategies. Furthermore, genetic counseling offers emotional support for individuals and families navigating the complex landscape of prostate cancer risk, helping to address concerns and provide guidance throughout the decision-making process.
What is prostate cancer?
Prostate cancer is a type of cancer that develops in the prostate gland, which is a small walnut-shaped gland that produces seminal fluid in males.
Why is it important to know your risk factors for prostate cancer?
Knowing your risk factors for prostate cancer is important because it can help you understand your likelihood of developing the disease and take appropriate preventive measures or early detection steps.
How does genetics play a role in prostate cancer?
Genetics can contribute to prostate cancer risk. Certain gene mutations or inherited gene variants can increase the likelihood of developing prostate cancer.
Can family history impact your prostate cancer risk?
Yes, having a family history of prostate cancer can increase your risk of developing the disease. If you have a close relative, such as a father or brother, who has had prostate cancer, your risk is higher.
How do genetic mutations influence prostate cancer risk?
Genetic mutations can increase the risk of prostate cancer by altering the functioning of genes involved in cell growth and division.
What is the link between inherited gene variants and prostate cancer?
Inherited gene variants, such as variants in the BRCA1 and BRCA2 genes, have been associated with an increased risk of prostate cancer.
Which specific genes are associated with prostate cancer risk?
In addition to BRCA1 and BRCA2, other genes such as HOXB13, CHEK2, and ATM have been identified as potential genetic risk factors for prostate cancer.
How do lifestyle choices impact prostate cancer risk?
Certain lifestyle choices, such as a healthy diet, regular exercise, and avoiding tobacco and excessive alcohol consumption, can help reduce the risk of prostate cancer.
What is the interaction between genetic and environmental factors in prostate cancer risk?
Genetic factors and environmental factors, such as diet and exposure to certain chemicals, can interact and influence prostate cancer risk. Understanding this interaction can help individuals make informed choices.
Why is regular screening important for prostate cancer?
Regular screening is important for detecting prostate cancer at its early stages when treatment is more effective. It can significantly increase the chances of successful treatment and survival.
What is the role of early detection in prostate cancer prevention?
Early detection of prostate cancer through regular screening allows for timely intervention, which can prevent the progression of the disease and potentially save lives.
What are the available testing options for prostate cancer?
Prostate-specific antigen (PSA) test, digital rectal exam (DRE), and imaging tests like ultrasound, MRI, or biopsy are some of the available testing options for prostate cancer.
What are the benefits of genetic counseling for prostate cancer risk assessment?
Genetic counseling can provide individuals with a better understanding of their genetic risk for prostate cancer, help them make informed decisions about preventive measures or screening, and offer emotional support throughout the process.