Medications That Promote Testicular Health And Fertility
Understanding Testicular Health and Fertility
Testicular health plays a crucial role in a man’s overall well-being, particularly when it comes to fertility. The testicles, also known as testes, are responsible for producing sperm and testosterone, the primary male sex hormone. Understanding the factors that can affect testicular health and fertility is essential for men who wish to optimize their reproductive potential.
Several factors can influence testicular health, including lifestyle choices, medical conditions, and environmental factors. Some common causes of testicular health and fertility issues include hormonal imbalances, infections, varicoceles (enlarged veins in the scrotum), and genetic disorders. Additionally, certain medications, chemotherapy, radiation therapy, and even excessive heat exposure can have a detrimental effect on testicular function. It is important for men to be aware of these potential factors and take proactive steps to maintain their testicular health.
In this video, Dr. Raman Tanwar talks about normal variations and testicular size as well as Testicular self-examination.
The Importance of Testicular Health for Fertility
The health of the testicles plays a crucial role in male fertility. Testicles, also known as testes, are responsible for producing sperm and testosterone, the primary male sex hormone. When the testicles are healthy, they can produce an adequate amount of sperm that is capable of fertilizing an egg. However, when testicular health is compromised, it can significantly impact a man’s fertility.
One of the key reasons why testicular health is important for fertility is because it directly affects sperm production. Sperm production, or spermatogenesis, occurs within the seminiferous tubules of the testicles. These tubules contain specialized cells called spermatogonia, which undergo a series of maturation stages to ultimately form mature spermatozoa. Any disruption in the testicular health can interfere with this intricate process, leading to a decrease in sperm production or poor sperm quality. Consequently, this can decrease the chances of successfully fertilizing an egg and achieving pregnancy.
Here’s a table highlighting the importance of testicular health and fertility:
| Importance of Testicular Health and Fertility | Key Considerations | Credible Source |
|---|---|---|
| Reproduction and Family Planning | Healthy testicular function is essential for successful reproduction and family planning. Issues with testicular health can impact fertility. | American Urological Association – Male Infertility |
| Hormonal Regulation | Testicles produce testosterone, a key hormone for male reproductive health, influencing libido, muscle mass, and overall well-being. | Mayo Clinic – Testosterone |
| Sperm Production and Quality | Testicles play a crucial role in sperm production. Maintaining healthy testicular function is vital for producing high-quality sperm necessary for conception. | American Society for Reproductive Medicine – Male Reproductive Health |
| Sexual Function | Testicular health is linked to sexual function, including libido and the ability to achieve and sustain erections. Issues with testicular health may impact sexual satisfaction. | Cleveland Clinic – Male Sexual Dysfunction |
| Emotional Well-being | Fertility concerns or issues with testicular health may affect a man’s emotional well-being, leading to stress and anxiety. Seeking support is essential. | Resolve: The National Infertility Association – Emotional Aspects of Infertility |
| Overall Health Indicators | Testicular health can be indicative of a man’s overall health. Regular check-ups and addressing any concerns promptly contribute to overall well-being. | Urology Care Foundation – Men’s Health |
| Prevention of Testicular Disorders | Maintaining a healthy lifestyle and seeking medical advice for any concerns can contribute to the prevention of testicular disorders and potential fertility issues. | Urology Care Foundation – Testicular Disorders |
Common Causes of Testicular Health and Fertility Issues
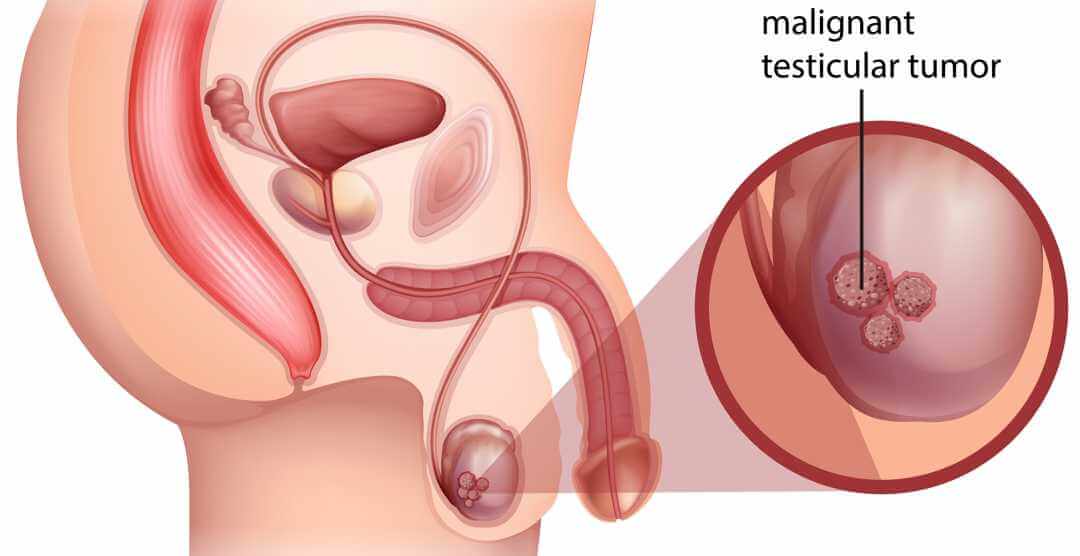
Testicular health and fertility issues can be influenced by a variety of factors, both biological and environmental. One common cause is hormonal imbalances, which can disrupt the delicate balance of testosterone and other hormones necessary for proper testicular function. Certain medical conditions, such as testicular cancer, undescended testicles, and varicoceles, can also contribute to testicular health and fertility problems.
Environmental factors can also play a significant role in testicular health and fertility issues. Exposure to certain chemicals, such as pesticides, heavy metals, and endocrine-disrupting substances, can have detrimental effects on the testicles and sperm production. Lifestyle choices, such as smoking, excessive alcohol consumption, and drug use, can further compound these issues. In addition, obesity and sedentary lifestyles have been linked to lower sperm quality and fertility problems.
Understanding the common causes of testicular health and fertility issues is crucial for both prevention and treatment. By addressing hormonal imbalances, managing medical conditions, and making lifestyle changes, men can take proactive steps to improve their reproductive health. Additionally, minimizing exposure to harmful chemicals and adopting a healthy diet and exercise routine can also have a positive impact. It is important for individuals experiencing fertility problems to consult with a healthcare professional to determine the underlying cause and appropriate treatment options. By taking control of their testicular health, men can increase their chances of achieving fertility and overall well-being.
Lifestyle Changes to Improve Testicular Health and Fertility

Maintaining good testicular health is essential for overall male fertility. By making certain lifestyle changes, men can significantly improve their chances of achieving healthy sperm production and reproductive function. Here are some key strategies to consider:
1. Quit smoking: Smoking has been linked to a decrease in sperm quality, motility, and count. The harmful chemicals in cigarettes can damage the DNA in sperm cells, leading to fertility problems. Quitting smoking is vital for enhancing testicular health and increasing the chances of successful conception.
2. Limit alcohol intake: Excessive alcohol consumption can have a detrimental effect on testicular health and fertility. It can disrupt hormone levels, decrease sperm production, and impair sperm quality. It is advisable to limit alcohol intake or abstain from it altogether to promote optimal reproductive function.
In addition to these lifestyle changes, other factors such as maintaining a healthy weight, managing stress levels, and avoiding exposure to environmental toxins can also play a role in improving testicular health and fertility. Taking proactive steps towards adopting a healthier lifestyle can lead to positive outcomes in terms of reproductive well-being.
The Role of Diet and Exercise in Testicular Health and Fertility

Maintaining a healthy lifestyle is crucial for optimal testicular health and fertility. Diet and exercise play a significant role in supporting the proper functioning of the male reproductive system. Research has shown that certain nutrients and dietary patterns can positively impact testicular health and enhance fertility.
A well-balanced diet rich in essential nutrients such as antioxidants, vitamins, minerals, and omega-3 fatty acids is essential for promoting testicular health. Antioxidants, found in fruits and vegetables, help protect sperm cells from oxidative stress and DNA damage. Foods high in vitamin C, such as citrus fruits and berries, have been shown to improve sperm quality. Similarly, vitamin E, found in nuts and seeds, can enhance sperm motility. Zinc, an important mineral for male fertility, is abundant in foods like oysters, beef, and pumpkin seeds. Including these nutrients in your diet can help maintain optimal testicular health and enhance fertility.
Natural Remedies and Supplements for Testicular Health and Fertility
There is growing interest in natural remedies and supplements that claim to improve testicular health and fertility. However, it is important to approach these options with caution and seek professional advice before incorporating them into your routine. While some studies suggest that certain herbs and supplements may have potential benefits, the evidence is still limited and more research is needed to establish their efficacy.
One natural remedy that has gained attention is Tribulus terrestris. This plant extract is commonly marketed as a testosterone booster and is believed to enhance sexual function and improve sperm quality. However, while some small-scale studies have shown positive effects, larger, more rigorous trials are needed to confirm these findings. It is also important to note that individual responses may vary, and Tribulus terrestris should not be considered a guaranteed solution for testicular health and fertility issues.
Another supplement that has been explored is Coenzyme Q10 (CoQ10). This compound is naturally produced by the body and plays a crucial role in energy production within cells. Some research suggests that CoQ10 supplementation may improve sperm quality and motility, making it a potential option for those experiencing fertility problems. However, further studies are needed to establish optimal dosages and potential side effects. It is always advisable to consult with a healthcare professional before starting any new supplement regimen.
Please note that while natural remedies and supplements may offer promising results, they should not replace or be solely relied upon as a substitute for medical advice. It is crucial to consult with a healthcare professional to determine the underlying causes of testicular health and fertility issues and to develop an appropriate treatment plan.
References:
1. Nagarajan N, et al. Efficacy of Tribulus terrestris on seminal parameters in men with subfertility: A crossover randomized clinical trial. Int J Reprod Biomed. 2016;14(12):743-748.
2. Safarinejad MR, et al. Coenzyme Q10 supplementation in infertile men with idiopathic asthenozoospermia: An open, randomized, placebo-controlled trial. Fertil Steril. 2012;98(3): S69-73.
– Tribulus terrestris is a natural remedy that is marketed as a testosterone booster and may improve sexual function and sperm quality.
– Limited studies have shown positive effects, but larger trials are needed to confirm these findings.
– Individual responses may vary, and it should not be considered a guaranteed solution for testicular health and fertility issues.
– Coenzyme Q10 (CoQ10) supplementation has been explored for improving sperm quality and motility.
– Further research is needed to establish optimal dosages and potential side effects of CoQ10 supplementation.
– Natural remedies and supplements should not replace medical advice or be solely relied upon for treatment.
References:
1. Nagarajan N, et al. Efficacy of Tribulus terrestris on seminal parameters in men with subfertility: A crossover randomized clinical trial. Int J Reprod Biomed. 2016;14(12):743-748.
2. Safarinejad MR, et al. Coenzyme Q10 supplementation in infertile men with idiopathic asthenozoospermia: An open, randomized, placebo-controlled trial. Fertil Steril. 2012;98(3): S69-73
The Impact of Stress on Testicular Health and Fertility

Stress is a pervasive aspect of modern life and its impact on overall health cannot be underestimated. When it comes to testicular health and fertility, the effects of stress can be particularly significant. Studies have shown that high levels of stress can have detrimental effects on male fertility by affecting sperm quality, quantity, and motility.
One way in which stress can affect testicular health is through hormonal imbalances. Stress triggers the release of cortisol, a hormone that can disrupt the delicate balance of reproductive hormones in the body. This can lead to a decrease in testosterone production, which is essential for healthy sperm development. Additionally, stress can cause oxidative stress in the body, leading to the production of reactive oxygen species (ROS) that can damage sperm DNA.
Furthermore, stress can also impact the quality of semen by affecting sperm movement. Research has shown that men who experience high levels of stress may have lower sperm motility, meaning that their sperm may have difficulty swimming towards the egg for fertilization. This can significantly reduce the chances of successful conception.
In conclusion, stress can have a profound effect on testicular health and fertility. It is important for men who are trying to conceive to prioritize stress management techniques, such as relaxation exercises, meditation, and engaging in hobbies or activities that bring joy and relaxation. By reducing stress levels, men can potentially improve their chances of achieving optimal testicular health and fertility.
Testicular Health and Fertility: Debunking Myths and Misconceptions
There are many myths and misconceptions surrounding testicular health and fertility. It is important to debunk these misconceptions in order to provide accurate information and promote better understanding of this topic.
One common misconception is that wearing tight underwear or pants can cause testicular health issues or fertility problems. However, there is no scientific evidence to support this claim. The temperature of the testicles is regulated by the body’s natural mechanisms, such as the cremaster muscle and the scrotum, which help to keep the testicles at an optimal temperature for sperm production.
Another myth is that masturbation can lead to infertility. This is not true. Masturbation is a normal sexual activity and is not linked to infertility. In fact, regular ejaculation through masturbation or sexual intercourse can help to improve sperm quality by preventing the build-up of old, damaged sperm.
It is important to dispel these myths and misconceptions in order to provide accurate information about testicular health and fertility. By understanding the facts, individuals can make informed decisions about their reproductive health and seek appropriate medical advice if needed.
Medical Treatments for Testicular Health and Fertility Issues
Medical Treatments for Testicular Health and Fertility Issues
When it comes to addressing testicular health and fertility issues, medical treatments are often sought to provide effective solutions. These treatments can vary depending on the underlying causes and severity of the condition. It is important to consult with a healthcare professional who specializes in reproductive medicine to determine the most appropriate course of action.
One common medical treatment for testicular health and fertility issues is hormone therapy. This involves the use of medications to address imbalances in hormone levels that may be affecting sperm production or the overall functioning of the testicles. Hormone therapy can help restore hormonal equilibrium and improve fertility outcomes. However, it is crucial to note that the use of hormone therapy should be carefully monitored by a healthcare provider to avoid potential side effects and ensure optimal results.
In situations where structural abnormalities or blockages are impeding the flow of sperm, surgical interventions may be recommended. Surgeries such as varicocele repair, vasectomy reversal, or sperm retrieval procedures can help restore or facilitate the proper movement of sperm. These surgical options can significantly improve fertility outcomes for individuals facing challenges in this area. However, as with any surgical intervention, there are potential risks and complications to consider. Therefore, it is crucial to thoroughly discuss the benefits and potential risks with a healthcare professional before deciding on the appropriate surgical approach.
In addition to these medical treatments, assisted reproductive technologies (ART) can also play a significant role in addressing testicular health and fertility issues. ART encompasses a range of procedures such as in-vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and intrauterine insemination (IUI). These techniques can assist individuals or couples in conceiving by bypassing certain fertility barriers and increasing the chances of successful fertilization. ART procedures are often performed by reproductive specialists and have shown promising results for individuals with various reproductive challenges.
It is important to note that the choice of medical treatment for testicular health and fertility issues will depend on the specific diagnosis, individual circumstances, and preferences. It is highly recommended to seek guidance from a healthcare professional who can assess the situation comprehensively and provide personalized advice. Additionally, maintaining a healthy lifestyle, adopting stress management strategies, and considering complementary approaches like acupuncture or herbal remedies may be beneficial in conjunction with medical treatments. Taking a holistic approach to testicular health and fertility can increase the chances of achieving desired outcomes and improving overall reproductive well-being.
Hormonal Therapies for Testicular Health and Fertility
Testicular health and fertility can be influenced by various factors, including hormonal imbalances. Hormonal therapies are often utilized as a treatment option for individuals experiencing testicular health and fertility issues. These therapies aim to restore hormonal balance, which is crucial for the proper functioning of the testes and the production of healthy sperm.
One commonly used hormonal therapy is testosterone replacement therapy (TRT). Testosterone is the primary male sex hormone and plays a vital role in the development and maintenance of testicular function. In cases where testosterone levels are low, TRT can help restore optimal hormone levels, leading to improved testicular health and fertility. However, it is essential to note that TRT should only be prescribed by a qualified healthcare professional after a thorough evaluation of the individual’s medical history and hormone levels.
Another hormonal therapy option used for testicular health and fertility issues is human chorionic gonadotropin (hCG) therapy. HCG is a hormone that stimulates the production of testosterone and promotes testicular health. It can be administered in injection form, and the dosage and frequency are determined based on the individual’s specific needs. HCG therapy has shown promising results in improving sperm production and quality, which can ultimately enhance fertility. However, as with any medical treatment, it is essential to consult with a healthcare professional to determine the suitability and potential risks of hCG therapy.
In conclusion, hormonal therapies such as testosterone replacement therapy and human chorionic gonadotropin therapy can be valuable tools in the management of testicular health and fertility issues. However, it is crucial to seek professional guidance and undergo comprehensive evaluations before starting any hormonal treatment. Each individual’s case is unique, and a personalized approach is necessary to achieve the best possible outcomes.
Surgical Options for Testicular Health and Fertility Problems
Surgical options for testicular health and fertility problems are available for individuals who experience more severe issues that cannot be addressed through lifestyle changes or medical treatments alone. These procedures aim to rectify underlying problems that may be hindering fertility or causing discomfort.
One common surgical option is varicocelectomy, which involves the removal or repair of varicocele veins in the scrotum. Varicoceles are enlarged veins that can cause pain, testicular shrinkage, and infertility. By surgically correcting the varicoceles, blood flow can be improved, potentially enhancing testicular health and fertility.
Another surgical procedure is testicular sperm extraction (TESE), which aims to retrieve sperm directly from the testes. This procedure is often recommended for men who have abnormalities in their sperm production or who have undergone previous unsuccessful attempts at sperm retrieval. TESE can be performed alongside other assisted reproductive technologies such as in vitro fertilization (IVF) to increase the chances of successful fertilization.
It is important to note that surgical options for testicular health and fertility problems should be considered on a case-by-case basis, with the guidance of a qualified healthcare professional. These procedures may carry risks and potential complications that should be thoroughly discussed and evaluated before making a decision. Additionally, the success rates and outcomes of these surgeries can vary depending on individual circumstances, highlighting the need for personalized treatment plans.
The Role of Assisted Reproductive Technologies in Testicular Health and Fertility
Assisted reproductive technologies (ART) have revolutionized the field of reproductive medicine, offering hope and options for couples facing testicular health and fertility issues. ART refers to the various techniques and procedures that assist in achieving pregnancy when natural conception is not possible. These technologies include in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and sperm and egg donation.
For couples where male factor infertility is the primary concern, ART can be particularly beneficial. In cases where there is a low sperm count, poor sperm motility, or abnormal sperm morphology, ART procedures can help overcome these barriers. Through IVF or ICSI, sperm can be directly injected into an egg, increasing the chances of fertilization and subsequent implantation in the uterus. This opens up the possibility of achieving a pregnancy that would not have been possible otherwise.
It is important to note that the decision to pursue ART should be made in consultation with a reproductive specialist, who can assess individual circumstances and provide personalized recommendations. As with any medical procedure, ART carries potential risks and considerations that need to be weighed against the desired outcome. It is crucial for couples to have a thorough understanding of the process, success rates, and associated costs before embarking on an ART journey.
In conclusion, assisted reproductive technologies play a significant role in addressing testicular health and fertility challenges. These technologies provide a ray of hope for couples by offering alternative means of conception. However, it is always advised to seek expert medical guidance and consider all factors before making a decision regarding ART. In the next section, we will explore the various psychological support options available to men coping with testicular health and fertility issues.
Psychological Support for Men Coping with Testicular Health and Fertility Issues
Psychological support plays a crucial role in helping men cope with testicular health and fertility issues. Dealing with such challenges can be emotionally overwhelming, causing stress, anxiety, and depression. It is essential to address these psychological aspects to provide comprehensive care to individuals experiencing difficulties with their reproductive health.
Men facing testicular health and fertility issues may experience a range of emotions, including feelings of inadequacy, shame, and loss. They may also have concerns about their masculinity and the impact these issues could have on their relationships and sense of self. Seeking professional psychological support can help individuals navigate these complex emotions and develop effective coping strategies. Therapy and counseling can provide a safe space for men to express their feelings, ask questions, and learn techniques to manage stress and anxiety associated with their condition.
It is important to note that psychological support should not be seen as a standalone treatment for testicular health and fertility issues, but rather as an integral part of a comprehensive approach. By addressing both the physical and emotional aspects, individuals can gain a better understanding of their condition and develop strategies to improve their overall well-being. In the next section, we will explore strategies to maintain testicular health and fertility in the long term, including lifestyle changes and medical treatments that can complement psychological support.
Maintaining Testicular Health and Fertility: Long-term Strategies
Maintaining testicular health and fertility requires a proactive approach that encompasses various aspects of a man’s lifestyle. One crucial long-term strategy is to prioritize regular exercise and physical activity. Engaging in moderate-intensity exercises, such as brisk walking, jogging, or cycling, can have a positive impact on testicular health and fertility by improving blood circulation to the reproductive organs and reducing the risk of obesity, which has been linked to decreased sperm quality and quantity.
Additionally, adopting a balanced and nutritious diet is paramount for maintaining testicular health and fertility. Including a diverse range of fruits, vegetables, whole grains, lean proteins, and healthy fats in your daily meals provides essential vitamins, minerals, and antioxidants that support sperm production and function. Conversely, a diet high in processed foods, saturated fats, and sugary beverages may adversely affect testicular health and fertility. It’s advisable to limit the consumption of alcohol, caffeine, and tobacco, as studies have shown that these substances can have detrimental effects on male reproductive function. A well-rounded diet should also incorporate an adequate intake of fluids to ensure proper hydration, which is essential for maintaining optimal testicular function.
What is testicular health and why is it important for fertility?
Testicular health refers to the overall well-being and proper functioning of the testicles. It is important for fertility because the testicles produce and store sperm, which is necessary for reproduction.
What are the common causes of testicular health and fertility issues?
Common causes include hormonal imbalances, genetic factors, infections, testicular trauma or injury, certain medical conditions, lifestyle choices, and environmental factors.
What lifestyle changes can improve testicular health and fertility?
Lifestyle changes such as maintaining a healthy weight, quitting smoking, limiting alcohol consumption, avoiding excessive heat to the testicles, and managing stress levels can improve testicular health and fertility.
How does diet and exercise affect testicular health and fertility?
A balanced diet that includes essential nutrients and antioxidants can support testicular health and fertility. Regular exercise improves blood flow to the testicles, which is beneficial for their overall function.
Are there any natural remedies or supplements that can improve testicular health and fertility?
Some natural remedies and supplements, such as maca root, zinc, selenium, and vitamins C and E, have been associated with improved testicular health and fertility. However, it is important to consult with a healthcare professional before starting any new supplements.
Can stress affect testicular health and fertility?
Yes, chronic stress can negatively impact testicular health and fertility by affecting hormone levels and sperm production. Managing stress through relaxation techniques and seeking support can help maintain testicular health.
What are some common myths and misconceptions about testicular health and fertility?
There are several myths and misconceptions surrounding testicular health and fertility, such as the belief that wearing tight underwear or using laptops on the lap can cause infertility. These claims have not been scientifically proven.
What medical treatments are available for testicular health and fertility issues?
Medical treatments for testicular health and fertility issues may include hormone replacement therapy, medications to treat infections or hormonal imbalances, and surgical interventions if necessary.
What are hormonal therapies used for testicular health and fertility?
Hormonal therapies, such as testosterone replacement therapy, can be utilized to address hormonal imbalances that may be affecting testicular health and fertility.
What surgical options are available to address testicular health and fertility problems?
Surgical options may include procedures to repair testicular trauma or injury, varicocele repair, or sperm retrieval techniques for assisted reproductive technologies.
How do assisted reproductive technologies assist in testicular health and fertility?
Assisted reproductive technologies, such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI), can help couples conceive by bypassing some fertility issues related to testicular health.
Is there psychological support available for men coping with testicular health and fertility issues?
Yes, there are psychological support options available, including counseling or therapy, to help men cope with the emotional and psychological impacts of testicular health and fertility issues.
What are some long-term strategies for maintaining testicular health and fertility?
Long-term strategies include adopting a healthy lifestyle, managing stress effectively, seeking regular medical check-ups, following recommended treatments, and staying informed about advancements in reproductive health.






