Prostate Cancer 101: Everything You Need to Know About Staging and Testing

What is Prostate Cancer?
Prostate cancer is a type of cancer that affects the prostate gland, which is a small walnut-shaped gland located below the bladder in men. This gland plays a crucial role in the reproductive system as it produces fluid that nourishes and transports sperm.
The development of prostate cancer occurs when there is an abnormal growth of cells within the prostate gland. These cancerous cells can multiply and form tumors, which can then invade nearby tissues or spread to other parts of the body.
Prostate cancer is one of the most common types of cancer in men, with a higher incidence in older age groups. While the exact cause of prostate cancer is not known, there are several risk factors that have been identified, including age, family history, ethnicity, and certain genetic mutations.
Understanding the nature of prostate cancer and its risk factors is essential for early detection and treatment. Regular screening and awareness of the signs and symptoms of prostate cancer play a vital role in improving outcomes for patients. Diagnostic tests, such as prostate-specific antigen (PSA) testing and digital rectal examination (DRE), are commonly used to detect prostate cancer and assess its stage.
In the upcoming sections, we will delve deeper into the risk factors associated with prostate cancer, the importance of early detection through regular screening, and the signs and symptoms that may indicate the presence of this disease. Additionally, we will explore the various diagnostic tests used to detect prostate cancer and assess its stage, as well as the different treatment options available for localized and advanced prostate cancer.
• Prostate cancer is a type of cancer that affects the prostate gland.
• The prostate gland is located below the bladder in men and produces fluid for sperm.
• Abnormal growth of cells within the prostate gland leads to the development of prostate cancer.
• Cancerous cells can form tumors and invade nearby tissues or spread to other parts of the body.
• Prostate cancer is more common in older age groups.
• Risk factors for prostate cancer include age, family history, ethnicity, and certain genetic mutations.
• Early detection through regular screening and awareness of signs and symptoms are crucial for improving outcomes.
• Diagnostic tests such as PSA testing and DRE are commonly used to detect prostate cancer.
• Treatment options vary depending on whether the cancer is localized or advanced.
Understanding the Risk Factors for Prostate Cancer
Prostate cancer is one of the most common types of cancer affecting men worldwide. It is important to understand the risk factors associated with this disease in order to identify potential preventive measures and ensure early detection. Age is one of the primary risk factors for prostate cancer, with the majority of cases occurring in men over the age of 65. Additionally, research has shown that men with a family history of prostate cancer are at a higher risk of developing the disease themselves. Genetic factors play a significant role in prostate cancer, and certain inherited gene mutations have been linked to an increased risk. While these risk factors cannot be changed, awareness of them can help in making informed decisions about regular screenings and healthcare management.
There are also several lifestyle factors that have been associated with an increased risk of prostate cancer. A diet high in red meat and processed foods, as well as low consumption of fruits and vegetables, has been found to be a risk factor for developing prostate cancer. Obesity and a sedentary lifestyle have also been linked to an increased risk. On the other hand, research suggests that a diet rich in fruits, vegetables, and whole grains, as well as regular physical activity, may help reduce the risk of prostate cancer. It is important to note that while these factors may influence the risk of developing prostate cancer, they do not guarantee the development of the disease. The interaction between genetics, lifestyle, and environmental factors remains complex and requires further investigation. Understanding these risk factors can assist healthcare professionals in providing appropriate recommendations to reduce the risk and improve overall prostate health.
Early Detection: Importance of Regular Screening

Regular screening for prostate cancer is crucial in the early detection and management of this disease. Prostate cancer is the most common cancer in men, with approximately 1 in 8 men being diagnosed during their lifetime. The incidence increases with age, making regular screening even more important for older men.
Screening involves the use of specific tests to detect prostate cancer in its early stages, even before symptoms become apparent. The two main screening tests are the prostate-specific antigen (PSA) blood test and the digital rectal examination (DRE). The PSA test measures the level of PSA, a protein produced by the prostate gland, in the blood. Elevated levels of PSA may indicate the presence of prostate cancer. On the other hand, the DRE involves a physical examination of the prostate gland. The healthcare provider inserts a gloved finger into the rectum to feel for any abnormalities in the size, shape, and texture of the prostate.
The combination of these screening tests provides a comprehensive evaluation of the prostate and helps identify men who may require further investigation. Early detection through regular screening offers several benefits, including a higher likelihood of successful treatment and the potential to prevent the spread of cancer to other parts of the body. By detecting prostate cancer in its early stages, treatment options such as surgery, radiation therapy, and active surveillance can be initiated promptly, leading to better outcomes for patients. Regular screening also allows healthcare providers to closely monitor individuals at higher risk due to factors such as family history or certain genetic mutations.
In conclusion, regular screening is essential for the early detection of prostate cancer. Through a combination of the PSA blood test and the DRE, healthcare providers can identify potential cases of prostate cancer and take appropriate action. Early detection offers benefits such as more treatment options and improved chances of successful outcomes. Men should discuss the possibility of prostate cancer screening with their healthcare providers and make an informed decision based on their individual risk factors and preferences.
Signs and Symptoms of Prostate Cancer
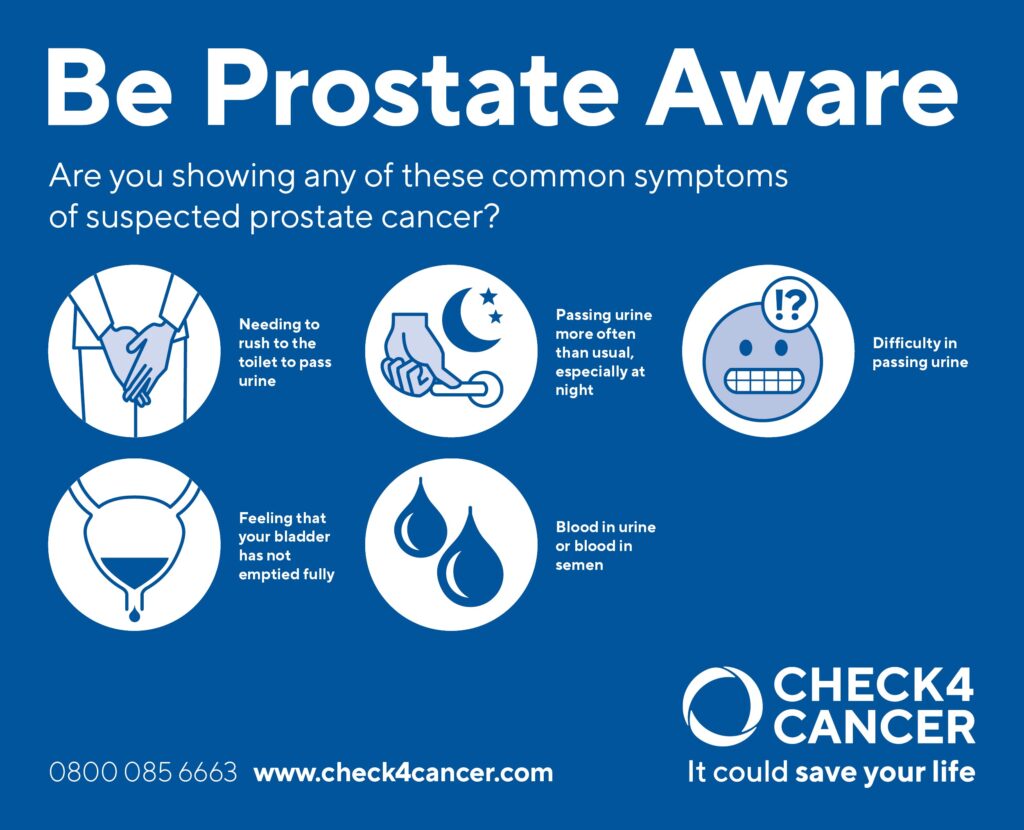
Prostate cancer is a prevalent cancer among men worldwide, and being familiar with its signs and symptoms is crucial for early detection and timely management. Often, in the early stages, prostate cancer does not cause any noticeable symptoms. However, as the disease progresses, certain signs may start to manifest.
One common symptom experienced by men with prostate cancer is urinary changes. These changes can include a weak or interrupted urine flow, frequent urination (especially at night), difficulty initiating or stopping urination, and a feeling of incomplete bladder emptying. Additionally, some individuals may experience blood in their urine or semen, which can be alarming. It is important to note that these symptoms can also be indicative of other non-cancerous conditions, such as benign prostatic hyperplasia (BPH). Therefore, it is essential to consult a healthcare professional for an accurate diagnosis and personalized treatment plan.
Diagnostic Tests for Prostate Cancer
Prostate cancer is a common form of cancer that affects men, particularly those who are older. It is important to note that not all prostate cancers are life-threatening, as some can grow slowly and may not require immediate treatment. However, diagnosing prostate cancer in its early stages is crucial for effective treatment and positive outcomes.
One of the main diagnostic tests used to detect prostate cancer is the prostate-specific antigen (PSA) test. PSA is a protein produced by the prostate gland, and elevated levels of this protein may indicate the presence of cancer or other conditions, such as an enlarged prostate. While the PSA test is a valuable tool in initial screening, it should be noted that elevated PSA levels are not always a definitive sign of prostate cancer. Other factors, such as age, race, and certain medications, can also influence PSA levels. By combining the PSA test with other diagnostic tests, such as a digital rectal exam (DRE) and a prostate biopsy, doctors can obtain a more accurate diagnosis and determine the appropriate course of action for their patients.
It is worth mentioning that not all prostate cancers require immediate treatment. Some men may be candidates for active surveillance, which involves closely monitoring the cancer with regular check-ups, PSA tests, and biopsies. This approach allows men to avoid potential side effects from aggressive treatments while still receiving appropriate care. However, it is important for patients to work closely with their healthcare providers to determine the best course of action based on their individual circumstances, including factors such as age, overall health, and the aggressiveness of the cancer. By utilizing various diagnostic tests and collaborating with medical professionals, individuals can make informed decisions regarding the management of prostate cancer.
Different Stages of Prostate Cancer
Prostate cancer is a complex disease that progresses in different stages. These stages help healthcare providers determine the extent and severity of the cancer, which is crucial in devising an effective treatment plan. Understanding the different stages can provide valuable insights into the progression and management of prostate cancer.
The initial stage, known as stage I, typically indicates that the cancer is localized within the prostate gland and is small in size. During this stage, the cancer cells are often slow-growing and may not cause any noticeable symptoms. As the disease progresses to stage II, the tumor may become larger but still remains confined within the prostate gland. At this point, the cancer may still be manageable and can be treated effectively.
Advancing to stage III, the cancer cells start to spread beyond the prostate gland and may invade nearby tissues or structures. In some cases, the cancer may spread to the seminal vesicles or lymph nodes. At this stage, the risk of the cancer becoming aggressive and spreading further increases significantly.
Stage IV is the most advanced stage of prostate cancer. The cancer cells have spread beyond the prostate gland and may have invaded distant organs, such as the bones, liver, or lungs. This stage is considered metastatic prostate cancer and is typically more difficult to treat. However, with advancements in treatment options and personalized approaches, healthcare providers can still offer viable treatment options to manage the disease and improve the quality of life for patients.
Understanding the different stages of prostate cancer helps doctors determine the best approach to treatment. It also plays a vital role in providing patients with valuable information about their condition and what to expect. In the following sections, we will delve further into the diagnostic tests and imaging techniques used to stage prostate cancer accurately, as well as the various treatment options available for each stage.
Certainly! Here’s a short data table on the different stages of prostate cancer:
| Stages of Prostate Cancer | Key Concepts | Credible Source |
|---|---|---|
| Stage I – Localized | – Key Concept: Cancer is confined to the prostate gland, often with slow growth and minimal symptoms. | American Cancer Society – Staging of Prostate Cancer |
| – Considerations: Prognosis is generally favorable, and treatment may include active surveillance, surgery, or radiation. | ||
| Stage II – Localized | – Key Concept: Cancer may be larger or more aggressive than in Stage I, but it is still confined to the prostate. | Cancer.net – Stages of Prostate Cancer |
| – Considerations: Treatment options may include surgery, radiation, or other localized therapies. | ||
| Stage III – Locally Advanced | – Key Concept: Cancer has spread beyond the prostate, possibly into nearby tissues, seminal vesicles, or lymph nodes. | Mayo Clinic – Prostate Cancer Stages |
| – Considerations: Treatment may involve a combination of surgery, radiation, and hormone therapy. | ||
| Stage IV – Advanced | – Key Concept: Cancer has spread to distant organs like bones, liver, or lungs, indicating advanced metastasis. | Cancer.gov – Prostate Cancer Stages |
| – Considerations: Treatment focuses on managing symptoms, with options like hormone therapy, chemotherapy, or immunotherapy. | ||
| Recurrent Prostate Cancer | – Key Concept: Cancer has returned after initial treatment, either locally or at distant sites. | American Cancer Society – Recurrent Prostate Cancer |
| – Considerations: Management may involve salvage therapies or a different approach based on the nature of recurrence. |
The Role of Imaging Techniques in Staging Prostate Cancer
Imaging techniques play a crucial role in accurately staging prostate cancer, providing valuable information for treatment planning and determining the best course of action for patients. One such imaging technique commonly used is magnetic resonance imaging (MRI). MRI scans are capable of producing detailed images of the prostate gland and surrounding structures, allowing medical professionals to assess the extent and location of the cancer. This information is vital in determining the appropriate treatment options and evaluating the potential spread of the disease.
Another imaging technique frequently employed in staging prostate cancer is computed tomography (CT) scanning. CT utilizes X-rays and computer processing to create cross-sectional images of the body. By visualizing the prostate and nearby lymph nodes, CT scans can help identify any abnormalities or metastases that may have occurred. Alongside MRI, this technique aids in accurately assessing the stage of the cancer and guiding treatment decisions. Moreover, positron emission tomography (PET) scans are also used in some cases to detect distant metastases, particularly in advanced or aggressive prostate cancer cases. The detailed information provided by these imaging techniques is indispensable in understanding the extent and progression of prostate cancer, enabling healthcare professionals to provide the most appropriate management strategies for patients.
Gleason Score: Assessing the Aggressiveness of Prostate Cancer
The Gleason score is a widely used system for assessing the aggressiveness of prostate cancer. It plays a crucial role in determining the appropriate treatment approach for patients. This score is determined by examining prostate tissue samples obtained through biopsy. The pathologist evaluates the samples under a microscope and assigns a grade to the cancer cells based on their appearance.
The Gleason score is composed of two grades, each ranging from 1 to 5. The primary grade represents the most common pattern of cancer cells observed, while the secondary grade represents the next most common pattern. These grades are then added together to yield the Gleason score, which can range from 2 to 10. A higher Gleason score indicates a more aggressive form of prostate cancer, while a lower score suggests a less aggressive or potentially indolent cancer. This information helps healthcare professionals make informed decisions regarding treatment options and prognosis.
Treatment Options for Localized Prostate Cancer
Treatment options for localized prostate cancer are varied and depend on several factors such as the stage and aggressiveness of the disease, overall health of the patient, and their personal preferences. The main treatment options for localized prostate cancer include active surveillance, surgery, radiation therapy, and focal therapy.
Active surveillance, also known as watchful waiting, is often recommended for patients with low-risk prostate cancer. This approach involves closely monitoring the cancer with regular check-ups and tests, and only initiating treatment if the cancer shows signs of progression. Active surveillance aims to avoid unnecessary treatment and its potential side effects, while still ensuring timely intervention if needed.
Surgery, specifically radical prostatectomy, involves the removal of the entire prostate gland. This procedure is typically recommended for patients with localized prostate cancer that has not spread beyond the gland. Depending on the individual case, the surgeon may perform an open surgery, laparoscopic surgery, or robot-assisted surgery. Surgery can be an effective treatment option, but it may carry risks such as urinary incontinence and erectile dysfunction. It is important for patients to discuss these potential side effects with their healthcare provider before making a decision.
Advanced Prostate Cancer: Treatment Approaches and Considerations
Advanced prostate cancer refers to cancer that has spread beyond the prostate gland to nearby tissues and organs or to distant parts of the body. When treating advanced prostate cancer, healthcare providers take into consideration various factors such as the extent of the cancer, the overall health of the patient, and the goals of treatment.
One common approach to managing advanced prostate cancer is hormone therapy, also known as androgen deprivation therapy (ADT). This treatment targets the male hormones, specifically testosterone, which can fuel the growth of prostate cancer cells. By decreasing the levels of testosterone in the body, hormone therapy aims to slow down the progression of the cancer and relieve symptoms. Hormone therapy can be administered through injections, pills, or implants and may be used alone or in combination with other treatments. Additionally, a newer form of hormone therapy called androgen receptor inhibitors has shown promising results in treating advanced prostate cancer, particularly in cases that have become resistant to traditional hormone therapy.
Another treatment option for advanced prostate cancer is chemotherapy. Chemotherapy involves the use of drugs to kill cancer cells and is typically administered intravenously. It is often used when the cancer has spread to distant parts of the body and cannot be effectively controlled by hormone therapy alone. Chemotherapy may also be combined with hormone therapy to maximize the effectiveness of treatment. Although chemotherapy can cause side effects such as fatigue, nausea, and hair loss, recent advancements in targeted therapies have helped to minimize these effects and improve overall outcomes for patients.
Managing Side Effects of Prostate Cancer Treatment
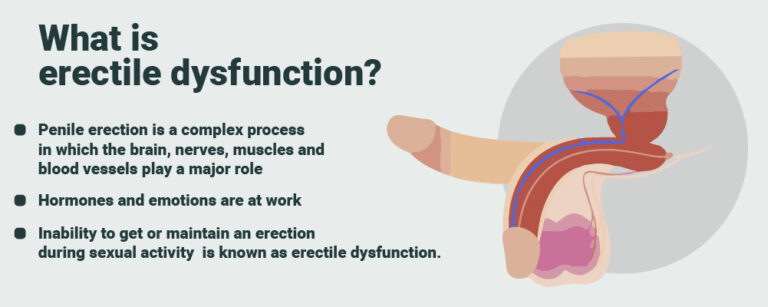
Managing the side effects of prostate cancer treatment is an important aspect of care for patients undergoing therapy. One common side effect of treatment is erectile dysfunction, which can significantly impact a man’s quality of life. Various treatment options such as medications, penile implants, and vacuum erection devices can help manage this side effect. It is essential for patients to discuss these options with their healthcare provider to determine the most suitable approach for them.
In addition to erectile dysfunction, urinary incontinence is another potential side effect of prostate cancer treatment. This can range from occasional leakage to complete loss of bladder control. Pelvic floor exercises, also known as Kegels, have been shown to be effective in improving urinary continence. These exercises target the muscles that support the bladder and can be performed anywhere, making them a convenient and accessible option for patients. Additionally, there are specialized absorbent products available that can help manage urinary leakage and provide comfort and confidence to individuals experiencing this side effect.
Supportive Care for Prostate Cancer Patients
Supportive care plays a crucial role in improving the quality of life for prostate cancer patients. It focuses on managing the physical, emotional, and psychological challenges that arise during and after treatment. Rehabilitation programs are often recommended to help patients regain their strength and mobility and alleviate any physical limitations caused by the disease or its treatment. These programs may include exercises, physical therapy, and occupational therapy to support patients in regaining their independence and improving their overall well-being.
In addition to physical rehabilitation, psychological support is equally important for prostate cancer patients. The diagnosis and treatment of prostate cancer can have a significant impact on a patient’s mental health, leading to anxiety, depression, or changes in body image. Counseling and support groups are valuable resources for patients and their families, providing a safe space to discuss their concerns and fears. These interventions can help patients cope with the emotional challenges of the disease, enhance their resilience, and promote a sense of empowerment throughout their journey.
As research continues to advance, the field of supportive care for prostate cancer patients is constantly evolving. New interventions, such as mindfulness-based stress reduction programs and cognitive-behavioral therapy, are showing promise in enhancing emotional well-being and reducing psychological distress. Furthermore, healthcare professionals are increasingly recognizing the importance of incorporating complementary approaches, such as acupuncture or yoga, into the supportive care plan to alleviate treatment-related side effects and improve overall quality of life. By providing comprehensive, patient-centered care, supportive care plays a vital role in helping prostate cancer patients navigate the challenges of their diagnosis and treatment, fostering physical and emotional healing along the way.
Lifestyle Changes to Reduce the Risk of Prostate Cancer
Lifestyle plays a crucial role in reducing the risk of prostate cancer. By adopting certain changes in daily habits and choices, men can potentially lower their chances of developing this disease. One of the key lifestyle factors to consider is maintaining a healthy diet. Studies have shown that consuming a diet rich in fruits, vegetables, whole grains, and lean proteins can have a protective effect against prostate cancer. These foods are abundant in essential nutrients, antioxidants, and phytochemicals, which possess anti-inflammatory properties and contribute to overall well-being.
In addition to a healthy diet, regular exercise is another important aspect of reducing the risk of prostate cancer. Engaging in moderate to vigorous physical activity for at least 150 minutes per week has been associated with a lower risk of developing this disease. Exercise not only helps in weight management but also improves overall cardiovascular health and enhances immune function, thereby potentially reducing the chances of cancer progression. It is advisable to incorporate a combination of aerobic activities, strength training, and flexibility exercises into one’s routine.
While lifestyle changes cannot guarantee complete protection against prostate cancer, they serve as a proactive step towards minimizing the risk. By adopting a nutritious diet and incorporating regular exercise into one’s daily routine, individuals can take charge of their health and potentially decrease their susceptibility to prostate cancer. It is essential to consult with healthcare professionals to customize an appropriate lifestyle plan based on individual needs and medical history.
Prostate Cancer Research and Future Developments
Recent advancements in prostate cancer research and future developments bring hope for improved diagnostics and treatments for this prevalent disease. Scientists have been focusing on various areas to enhance early detection methods and refine treatment options. One promising avenue of research involves the identification of novel biomarkers that can aid in the detection and monitoring of prostate cancer. These biomarkers, such as prostate-specific antigen (PSA) and genetic markers, offer a more targeted approach to screening and can provide valuable information about the aggressiveness of the cancer.
Furthermore, ongoing studies are investigating the role of imaging techniques in staging prostate cancer. Advanced imaging modalities, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), are being utilized to visualize the extent of the disease and determine the most appropriate treatment approach. These innovative imaging techniques not only improve the accuracy of staging but also help in guiding biopsies and monitoring treatment response.
In addition to these advancements, researchers are exploring new treatment approaches for advanced prostate cancer. Immunotherapy, for instance, has shown promise in stimulating the body’s immune system to target prostate cancer cells. Targeted therapies, which aim to inhibit specific molecules involved in cancer growth, are also being developed to improve treatment outcomes. Clinical trials are underway to evaluate the efficacy and safety of these novel therapies, offering patients a potential alternative when standard treatment options fail.
Prostate cancer research continues to evolve rapidly as scientists strive for a comprehensive understanding of the disease and seek innovative ways to tackle it. By staying abreast of the latest developments and investing in further research, we can hope for breakthroughs that will ultimately lead to better outcomes and improved quality of life for prostate cancer patients.
What is prostate cancer?
Prostate cancer is a type of cancer that develops in the prostate gland, which is a part of the male reproductive system.
What are the risk factors for prostate cancer?
Risk factors for prostate cancer include age, family history, race, certain genetic mutations, and lifestyle factors such as diet and exercise.
Why is early detection of prostate cancer important?
Early detection of prostate cancer is important because it increases the chances of successful treatment and improves survival rates.
What are the signs and symptoms of prostate cancer?
Common signs and symptoms of prostate cancer include urinary problems, such as frequent urination, weak urine flow, blood in the urine, and erectile dysfunction.
What diagnostic tests are used for prostate cancer?
Diagnostic tests for prostate cancer include a prostate-specific antigen (PSA) blood test, digital rectal exam (DRE), prostate biopsy, and imaging techniques such as MRI, CT scan, or bone scan.
What are the different stages of prostate cancer?
Prostate cancer is staged based on the size and extent of the tumor, whether it has spread to nearby tissues or lymph nodes, and if it has metastasized to distant organs.
How do imaging techniques help in staging prostate cancer?
Imaging techniques such as MRI, CT scan, and bone scan can help determine the extent of prostate cancer by visualizing the prostate gland and identifying any spread to surrounding tissues or distant sites.
What is the Gleason score and why is it important?
The Gleason score assesses the aggressiveness of prostate cancer by examining the patterns of cancer cells in a biopsy sample. It helps guide treatment decisions and predict prognosis.
What are the treatment options for localized prostate cancer?
Treatment options for localized prostate cancer may include active surveillance, surgery (prostatectomy), radiation therapy, or brachytherapy.
How are advanced prostate cancer cases treated?
Treatment approaches for advanced prostate cancer may include hormone therapy, chemotherapy, targeted therapy, immunotherapy, or radiation therapy to manage symptoms and slow the progression of the disease.
How can the side effects of prostate cancer treatment be managed?
Side effects of prostate cancer treatment, such as urinary incontinence, erectile dysfunction, and fatigue, can be managed through various interventions such as medications, lifestyle modifications, and support from healthcare professionals.
What supportive care options are available for prostate cancer patients?
Supportive care for prostate cancer patients may include pain management, psychological support, nutritional guidance, and palliative care to improve quality of life during and after treatment.
What lifestyle changes can reduce the risk of prostate cancer?
Making healthy lifestyle choices such as maintaining a balanced diet, engaging in regular physical activity, avoiding tobacco and excessive alcohol consumption, and managing stress can help reduce the risk of prostate cancer.
What are the current research and future developments in prostate cancer?
Ongoing research in prostate cancer focuses on improving screening methods, developing targeted therapies, exploring immunotherapy options, and investigating genetic factors to better understand the disease and improve treatment outcomes.