Prostate Cancer: Important Facts Every Man Needs to Know

Risk factors for prostate cancer
Age is one of the most significant risk factors for prostate cancer. The chances of developing prostate cancer increase as men grow older, with the majority of cases diagnosed in men over the age of 65. According to a study published in the Journal of Clinical Oncology, the incidence rate of prostate cancer in men aged 75 years or older is approximately 10 times higher than that in men aged 55 to 64. While the exact reason behind this age association is not fully understood, it is believed to be related to cumulative exposure to potential carcinogens and genetic changes that occur over time.
Another risk factor for prostate cancer is a family history of the disease. Men with a first-degree relative, such as a father or brother, who has been diagnosed with prostate cancer are at a higher risk themselves. A study conducted by the National Cancer Institute found that the risk of developing prostate cancer is approximately twice as high for men with an affected father or brother compared to those without a family history. This suggests a possible genetic component to the development of prostate cancer. However, it is important to note that having a family history does not guarantee that a man will develop prostate cancer, but rather increases the likelihood.
• Age is a significant risk factor for prostate cancer, with the majority of cases diagnosed in men over the age of 65.
• The incidence rate of prostate cancer in men aged 75 years or older is approximately 10 times higher than that in men aged 55 to 64.
• Cumulative exposure to potential carcinogens and genetic changes over time may contribute to the increased risk with age.
• Family history of prostate cancer is another risk factor for developing the disease.
• Men with a first-degree relative, such as a father or brother, who has been diagnosed with prostate cancer are at a higher risk themselves.
• The risk of developing prostate cancer is approximately twice as high for those with an affected father or brother compared to those without a family history.
Note: Having a family history does not guarantee that a man will develop prostate cancer but increases the likelihood.
Signs and symptoms of prostate cancer
Prostate cancer is a condition that affects the prostate gland, a small walnut-shaped gland located in the male reproductive system. While it can be a slow-growing cancer, it is important to be aware of the signs and symptoms, as early detection can significantly impact the prognosis.
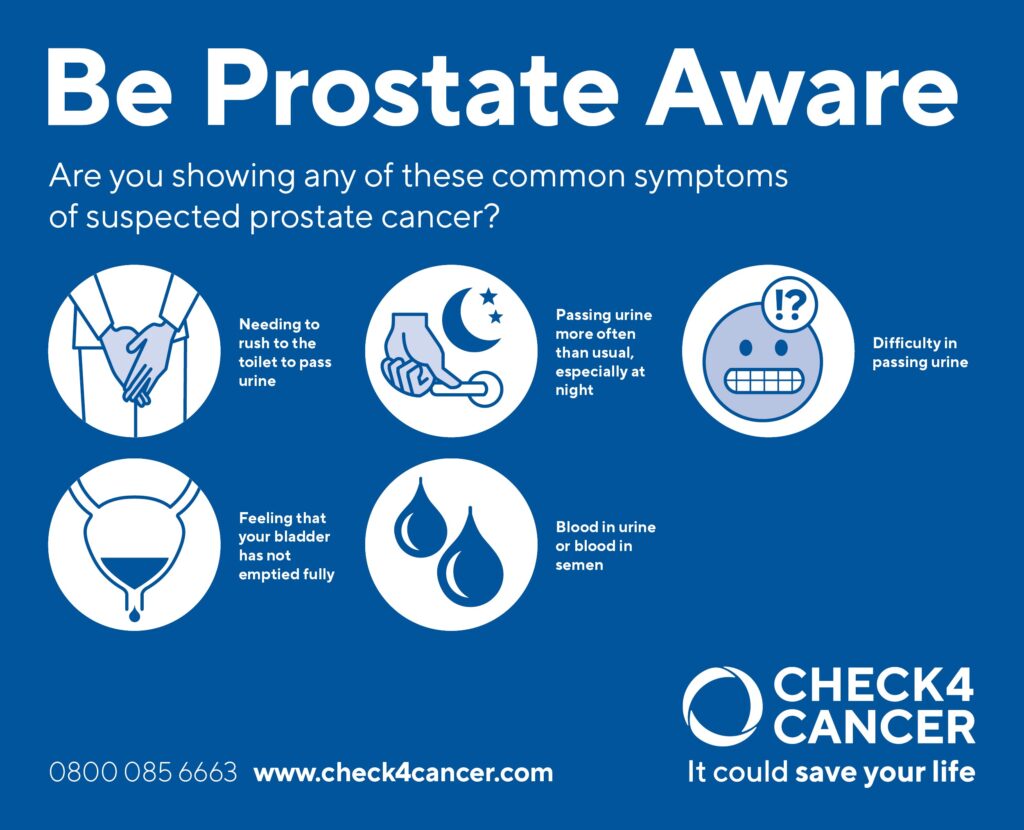
One of the most common symptoms of prostate cancer is difficulty in urination. This can include a weak urine flow, frequent urination, especially during the night, and the feeling of not being able to completely empty the bladder. Additionally, men may experience blood in the urine or semen, as well as discomfort or pain in the pelvic area. It is crucial to note that these symptoms can also be caused by benign conditions, such as an enlarged prostate or urinary tract infections. Therefore, if any of these signs persist or worsen, it is important to consult a healthcare professional for further evaluation.
While recognizing the signs and symptoms of prostate cancer is important, it is equally vital to understand the risk factors associated with the disease. Age is a significant factor, with the risk increasing as men get older, particularly after the age of 50. Family history and genetics also play a role, as having a first-degree relative with prostate cancer increases the likelihood of developing the disease. Other risk factors include race, with African-American men having a higher incidence, and certain lifestyle factors, such as a diet high in red meat and low in fruits and vegetables. By understanding both the signs and symptoms and the risk factors, men can take steps towards early detection and improved outcomes.
The importance of early detection
Prostate cancer is the second most common cancer among men worldwide. While the exact causes of prostate cancer are still not fully understood, there are several risk factors that have been identified. These include age, family history, race, and certain genetic mutations. Early detection is crucial in the successful treatment of prostate cancer, as it can help identify the disease at its earlier, more treatable stages.
Early detection of prostate cancer is primarily done through regular screening tests, such as the prostate-specific antigen (PSA) blood test and a digital rectal exam (DRE). These tests can help detect any abnormalities or changes in the prostate that may indicate the presence of cancer. It is important for men to discuss the benefits and limitations of these screening methods with their healthcare providers, as well as understand their individual risk factors, in order to make informed decisions about when to start screening and how often to repeat the tests. By detecting prostate cancer early, men have a better chance of receiving timely and appropriate treatment, improving their overall prognosis.
Here’s a short data table on the importance of early detection:
| Importance of Early Detection | Key Concepts | Credible Source |
|---|---|---|
| Increased Treatment Options | – Key Concept: Early detection allows for a wider range of treatment options and potentially less aggressive interventions. | American Cancer Society – Early Detection |
| – Considerations: Timely identification enhances the likelihood of successful treatment outcomes. | ||
| Improved Treatment Success | – Key Concept: Detecting cancer at an early stage often leads to more successful treatment and better long-term prognosis. | National Cancer Institute – Importance of Early Detection |
| – Considerations: Early intervention may result in a higher chance of a cure or long-term control of the disease. | ||
| Reduced Treatment Complexity | – Key Concept: Early detection may reduce the need for extensive treatments, minimizing potential side effects and complications. | Prostate Cancer Foundation – Early Detection |
| – Considerations: Identifying cancer early often allows for less invasive and more targeted treatment approaches. | ||
| Increased Survival Rates | – Key Concept: Early detection is associated with higher survival rates, emphasizing the importance of regular screenings. | Cancer.net – Prostate Cancer Early Detection |
| – Considerations: Regular screenings contribute to the overall improvement of survival outcomes. |
Common diagnostic tests for prostate cancer

Prostate cancer is one of the most common cancers found in men, and early detection is crucial for successful treatment outcomes. To diagnose prostate cancer, a combination of different tests and procedures is typically performed. These diagnostic tests help doctors assess the size and location of the tumor, as well as determine the stage and aggressiveness of the cancer.
One of the most commonly used tests for diagnosing prostate cancer is the prostate-specific antigen (PSA) blood test. PSA is a protein produced by cells in the prostate gland, and elevated levels of PSA can indicate the presence of prostate cancer. However, it’s important to note that an elevated PSA level does not necessarily mean cancer is present. Other conditions, such as an enlarged prostate or an infection, can also cause PSA levels to rise. Therefore, additional tests may be required to confirm a prostate cancer diagnosis. These tests can include a digital rectal examination (DRE), transrectal ultrasound (TRUS), and a prostate biopsy, where a small sample of tissue is taken for laboratory analysis.
In conclusion, a variety of diagnostic tests are available to detect and diagnose prostate cancer. These tests, such as the PSA blood test and prostate biopsy, provide valuable information about the presence and aggressiveness of the cancer. It’s important for men to regularly monitor their prostate health and discuss any concerns with their healthcare provider, as early detection greatly improves the chances of successful treatment.
Understanding the different stages of prostate cancer
Prostate cancer is a complex disease that progresses through various stages, each with different characteristics and treatment options. Understanding these stages is crucial for patients and their healthcare providers to make informed decisions about the most appropriate course of action.
The first stage of prostate cancer is known as localized cancer, where the tumor is confined to the prostate gland. This stage often has no symptoms and may be detected through routine screening or during investigations for other prostate-related issues. Treatment options for localized cancer may include active surveillance, where the tumor is monitored closely for any changes, or localized treatments such as surgery, radiation therapy, or focal therapy. The choice of treatment will depend on factors such as the patient’s age, overall health, and personal preferences.
As prostate cancer progresses, it may enter a more advanced stage called locally advanced cancer. In this stage, the tumor has spread beyond the prostate gland, but it has not yet reached distant organs. Common treatment options for locally advanced cancer include radiation therapy, hormone therapy, and sometimes surgery. It is important to note that treatment decisions for locally advanced cancer should be made in collaboration with a multidisciplinary team of healthcare professionals to ensure the best possible outcome for the patient.
Treatment options for prostate cancer
Prostate cancer is the most common cancer among men, second only to skin cancer. When it comes to treatment options for prostate cancer, several factors are taken into consideration, including the stage of the cancer, the overall health of the patient, and the potential side effects of each treatment. Some of the common treatment options for prostate cancer include active surveillance, surgery, radiation therapy, hormone therapy, and chemotherapy.
Active surveillance, also known as watchful waiting, is often recommended for men with low-risk prostate cancer. This approach involves regular monitoring of the cancer through PSA blood tests, digital rectal exams, and periodic biopsies. It is a suitable option for men with slow-growing tumors that are not causing any symptoms or posing a significant risk to their health.
Surgery, also called radical prostatectomy, involves the removal of the entire prostate gland and some surrounding tissue. This procedure can be done through open surgery or minimally invasive techniques such as laparoscopic or robotic-assisted surgery. Surgery is most effective for prostate cancer that is localized and has not spread beyond the prostate gland.
Radiation therapy uses high-energy X-rays or other types of radiation to kill cancer cells or stop them from growing. It can be delivered externally, through a machine that aims radiation at the prostate, or internally, through implants. Radiation therapy may be used as the primary treatment for localized prostate cancer or as a part of the treatment plan for more advanced cases.
Hormone therapy, also known as androgen deprivation therapy, aims to reduce the levels of testosterone in the body, as prostate cancer cells depend on this hormone for growth. This can be achieved through medication that blocks the production or action of testosterone, or by surgically removing the testicles. Hormone therapy is often used in combination with other treatments to enhance their effectiveness or to control cancer that has spread beyond the prostate.
Chemotherapy is mostly used in advanced cases of prostate cancer when the cancer has spread to other parts of the body. It involves the use of drugs that target and kill rapidly dividing cells, including cancer cells. Chemotherapy can help shrink tumors, relieve symptoms, and improve overall survival in some cases.
It is important to note that each treatment option has its own benefits and potential side effects. The choice of treatment depends on various factors, including the stage and aggressiveness of the cancer, the patient’s overall health, and their personal preferences. It is crucial for men diagnosed with prostate cancer to have an open and honest discussion with their healthcare team to understand the treatment options available to them and make an informed decision.
The role of surgery in treating prostate cancer
Prostate cancer, one of the most common types of cancer among men, can be treated in various ways. Surgery is often recommended as a primary treatment option for localized prostate cancer. The goal of surgery is to remove the entire prostate gland, along with any cancerous cells that may be present.
There are different surgical procedures available for treating prostate cancer, including radical prostatectomy and robotic-assisted laparoscopic prostatectomy. During a radical prostatectomy, the surgeon removes the entire prostate gland, along with surrounding tissues and lymph nodes if necessary. This procedure is typically performed using a traditional open surgery approach. On the other hand, robotic-assisted laparoscopic prostatectomy involves the use of a surgical robot to assist the surgeon in performing the procedure with smaller incisions. This minimally invasive approach often results in less blood loss, shorter hospital stays, and faster recovery times for patients.
Both types of prostate cancer surgeries have their own advantages and disadvantages, and the choice of procedure depends on factors such as the stage of the cancer, the patient’s overall health, and the surgeon’s expertise. It is important for patients to discuss the available options with their healthcare team to make an informed decision about the most appropriate surgical approach for their individual case.
The effectiveness of radiation therapy for prostate cancer
Radiation therapy is one of the primary treatment options for men diagnosed with prostate cancer. It involves the use of high-energy radiation beams to destroy cancer cells and shrink tumors. The effectiveness of radiation therapy in treating prostate cancer has been well-documented in numerous studies. Research has shown that radiation therapy can effectively eradicate cancer cells, particularly in early-stage prostate cancer cases. Additionally, it has been found to be equally as effective as surgery in terms of long-term cancer control.
One advantage of radiation therapy is its ability to specifically target the prostate gland while minimizing damage to surrounding healthy tissues. This precision is achieved through advanced technologies such as intensity-modulated radiation therapy (IMRT) and brachytherapy. IMRT allows for the delivery of high doses of radiation to cancerous cells while minimizing exposure to nearby organs, such as the bladder and rectum. Brachytherapy, on the other hand, involves placing small radioactive seeds directly inside the prostate, allowing for highly localized treatment. These techniques not only increase the effectiveness of radiation therapy but also reduce the risk of adverse side effects.
In conclusion, radiation therapy has proven to be an effective treatment option for prostate cancer. Its ability to selectively target cancer cells, along with advancements in technology, has made it a viable choice for many men diagnosed with this disease. However, it is important for patients to consult with their healthcare providers to determine the most appropriate treatment plan based on their individual circumstances. Further research and clinical trials continue to improve the understanding and effectiveness of radiation therapy in prostate cancer management.
Hormone therapy as a treatment option for prostate cancer
Prostate cancer is a common form of cancer in men, and hormone therapy is often used as a treatment option. Hormone therapy works by reducing the levels of testosterone in the body, as prostate cancer cells rely on testosterone to grow. By suppressing testosterone, hormone therapy can slow down the growth and spread of prostate cancer.
There are different types of hormone therapy available for prostate cancer, including luteinizing hormone-releasing hormone (LHRH) analogs, anti-androgens, and androgen deprivation therapy (ADT). LHRH analogs, such as leuprolide and goserelin, work by preventing the production of testosterone in the testicles. Anti-androgens, such as bicalutamide and flutamide, block the effects of testosterone in the body. ADT combines both LHRH analogs and anti-androgens to further reduce testosterone levels.
While hormone therapy can be effective in treating prostate cancer, it is not without its side effects. Common side effects may include hot flashes, sexual dysfunction, weight gain, and decreased bone density. It is important for patients to discuss these potential side effects with their healthcare provider and explore strategies to manage them effectively. Regular monitoring and follow-up appointments will also be necessary to track the effectiveness of hormone therapy and make any necessary adjustments to the treatment plan.
The potential side effects of prostate cancer treatments
Prostate cancer treatments can have various side effects, affecting the overall well-being of men undergoing these therapies. One potential side effect is erectile dysfunction (ED), which can occur after surgery, radiation therapy, or hormone therapy. Surgical procedures like radical prostatectomy can damage the nerves responsible for sexual function, leading to difficulties in achieving or maintaining an erection. Similarly, radiation therapy can also damage these nerves, causing ED as a long-term effect. Hormone therapy, which aims to reduce the production of testosterone, can lead to a decrease in sex drive and erectile function.
Another potential side effect of prostate cancer treatments is urinary incontinence. After surgery, some men may experience leakage or inability to control their urine flow. This can be a temporary or long-term side effect depending on the individual and the type of surgery performed. Additionally, radiation therapy can irritate the bladder and lead to urinary problems such as frequent urination or urgency. These side effects can significantly impact a man’s quality of life, affecting his self-esteem and daily activities. Therefore, it is crucial for healthcare providers to inform patients about these potential side effects and provide support and resources to manage them effectively.
The importance of regular follow-up appointments after treatment
After undergoing treatment for prostate cancer, it is crucial for patients to schedule regular follow-up appointments with their healthcare providers. These appointments play a vital role in monitoring the progress of the treatment and detecting any potential recurrence or side effects. Regular follow-up visits allow doctors to assess the overall health of the patient and provide necessary support and guidance during the recovery process.
During these appointments, healthcare providers may conduct a physical examination, perform relevant diagnostic tests, and discuss any concerns or symptoms the patient may be experiencing. Regular check-ups enable doctors to closely monitor the effectiveness of the treatment, assess the patient’s response to medications or therapies, and make any necessary adjustments to the treatment plan. In addition to the physical aspect, these appointments provide an opportunity for patients to discuss their emotional well-being and receive the necessary support and counseling to navigate through the challenges of post-treatment recovery. By prioritizing regular follow-up appointments, patients can ensure that they are receiving comprehensive and personalized care to manage their prostate cancer journey effectively.
Lifestyle changes that can help prevent prostate cancer
Lifestyle choices play a crucial role in preventing prostate cancer. Making certain modifications to your daily routine and habits can significantly reduce your risk of developing this disease. One important aspect is maintaining a healthy and balanced diet. Incorporating foods rich in antioxidants, such as fruits, vegetables, and whole grains, can provide protective benefits. Additionally, including sources of omega-3 fatty acids, such as fish like salmon and trout, in your diet may also be beneficial. Several studies have shown that these dietary modifications can help lower the risk of prostate cancer development.
Apart from dietary changes, regular exercise is equally important in reducing the risk of prostate cancer. Engaging in physical activity for at least 150 minutes per week, such as brisk walking, swimming, or cycling, can help maintain a healthy weight and lower the risk of developing prostate cancer. It is crucial to note that the intensity of exercise plays a significant role as well. High-intensity workouts may provide additional benefits in reducing the risk of prostate cancer compared to moderate or low-intensity exercises. Therefore, incorporating regular exercise into your routine is a vital step towards prostate cancer prevention.
The role of genetics in prostate cancer
Prostate cancer is a complex disease that can be influenced by both genetic and environmental factors. While the exact role of genetics in prostate cancer is still being studied, research has shown that having a family history of the disease can increase a man’s risk. In fact, men with a first-degree relative (such as a father or brother) who has been diagnosed with prostate cancer are at a higher risk themselves compared to those with no family history. Studies have also identified certain gene mutations that may be associated with an increased risk of developing prostate cancer. However, it is important to note that having these genetic variants does not necessarily mean that a man will develop the disease, as other factors play a role as well.
In addition to family history and gene mutations, researchers are also exploring the influence of other genetic factors, such as variations in certain genes that regulate hormone levels. Hormones, including testosterone and estrogen, have been implicated in the development and growth of prostate cancer. By understanding how these genes interact with hormones, scientists hope to gain insights into potential targets for prevention and treatment strategies. However, it is important to acknowledge that genetic factors are just one piece of the puzzle when it comes to prostate cancer, and more research is needed to fully understand their role and implications. By continuing to explore the genetic underpinnings of prostate cancer, scientists aim to develop personalized approaches to prevention, early detection, and treatment for men at risk.
Support resources for men with prostate cancer
Prostate cancer is a significant health concern for many men, and it can have a significant impact on their overall well-being. Fortunately, there are a variety of support resources available to men who have been diagnosed with prostate cancer, as well as to their loved ones. These resources aim to provide emotional support, education, and practical guidance throughout the journey of managing this condition.
One valuable support resource for men with prostate cancer is support groups. These groups provide a safe space for men to share their experiences, learn from others who have faced similar challenges, and gain valuable emotional support. Support groups can be in-person or online, offering individuals the opportunity to choose the format that works best for their needs. They often involve discussions led by healthcare professionals or experienced facilitators, providing relevant information about treatment options, managing side effects, and coping with the emotional impact of prostate cancer.
Additionally, many organizations and healthcare institutions offer educational programs and workshops focused on prostate cancer. These resources aim to provide individuals with a better understanding of the condition, its treatment options, and strategies for managing its physical and emotional effects. Education programs may cover topics such as nutrition, exercise, and lifestyle modifications that can support overall well-being during and after prostate cancer treatment. These programs often incorporate input from medical experts, ensuring that participants receive accurate and up-to-date information.
What are the risk factors for prostate cancer?
While the exact cause of prostate cancer is unknown, there are several risk factors that may increase a man’s chances of developing the disease. These include age (risk increases with age), family history of prostate cancer, certain genetic mutations, race (African-American men have a higher risk), and certain lifestyle factors such as a high-fat diet and lack of exercise.
What are the signs and symptoms of prostate cancer?
In the early stages, prostate cancer may not cause any noticeable signs or symptoms. As the disease progresses, symptoms may include difficulty urinating, frequent urination, blood in the urine or semen, erectile dysfunction, pain or discomfort in the pelvic area, and bone pain.
Why is early detection important in prostate cancer?
Early detection of prostate cancer is crucial because it increases the chances of successful treatment and better outcomes. Regular screenings and early diagnosis can help identify the disease at an early stage when it is more likely to be localized and easier to treat.
What are the common diagnostic tests for prostate cancer?
Common diagnostic tests for prostate cancer include a digital rectal exam (DRE), a prostate-specific antigen (PSA) blood test, and a prostate biopsy. These tests help evaluate the health of the prostate and determine if further investigation is needed.
What are the different stages of prostate cancer?
Prostate cancer is typically categorized into different stages based on the extent of the disease. The stages range from I to IV, with stage I being localized to the prostate and stage IV indicating cancer that has spread to other parts of the body.
What are the treatment options for prostate cancer?
Treatment options for prostate cancer depend on various factors such as the stage of the disease, overall health of the patient, and personal preferences. Common treatment options include active surveillance, surgery, radiation therapy, hormone therapy, chemotherapy, and immunotherapy.
What is the role of surgery in treating prostate cancer?
Surgery, such as a radical prostatectomy, is a common treatment option for localized prostate cancer. It involves the surgical removal of the prostate gland to eliminate the cancer cells. Surgery may be performed using traditional open surgery or minimally invasive techniques such as laparoscopic or robotic-assisted surgery.
How effective is radiation therapy for prostate cancer?
Radiation therapy is a common treatment for prostate cancer, particularly for localized or locally advanced disease. It uses high-energy X-rays to target and kill cancer cells. Radiation therapy can be delivered externally (external beam radiation) or internally (brachytherapy). Its effectiveness depends on the stage of cancer and individual circumstances.
Can hormone therapy be used as a treatment option for prostate cancer?
Yes, hormone therapy (also known as androgen deprivation therapy) is often used as a treatment option for advanced prostate cancer. It aims to lower the levels of male hormones (androgens) in the body, which can help slow down the growth of prostate cancer cells and alleviate symptoms.
What are the potential side effects of prostate cancer treatments?
The potential side effects of prostate cancer treatments vary depending on the type of treatment. Common side effects may include urinary incontinence, erectile dysfunction, bowel problems, fatigue, hot flashes, and hormonal changes. It is important to discuss potential side effects with healthcare providers before undergoing treatment.
Why are regular follow-up appointments important after prostate cancer treatment?
Regular follow-up appointments are important after prostate cancer treatment to monitor any potential recurrence, manage side effects, and ensure overall well-being. These appointments allow healthcare providers to assess the effectiveness of treatment and address any concerns or complications that may arise.
What lifestyle changes can help prevent prostate cancer?
While there is no guaranteed way to prevent prostate cancer, certain lifestyle changes may lower the risk. These include maintaining a healthy diet rich in fruits and vegetables, exercising regularly, maintaining a healthy weight, limiting the consumption of red meat and high-fat foods, and avoiding tobacco and excessive alcohol consumption.
What is the role of genetics in prostate cancer?
Genetics can play a role in prostate cancer. Having a family history of the disease, especially in a first-degree relative like a father or brother, can increase the risk. Additionally, certain inherited gene mutations, such as BRCA1 and BRCA2, have been associated with an increased risk of prostate cancer. Genetic counseling may be recommended for individuals with a strong family history or known genetic mutations.
Are there support resources available for men with prostate cancer?
Yes, there are numerous support resources available for men with prostate cancer. These can include support groups, online communities, counseling services, educational materials, and organizations dedicated to providing information and support for individuals and their families affected by prostate cancer. It is important to reach out and utilize these resources to help navigate the journey of prostate cancer.






